General Pediatrics 3
Session: General Pediatrics 3
222 - Novel implementation of caregiver fruit and vegetable intake quantification at a public hospital's pediatric primary care clinic: Implications for dyadic nutritional intervention
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 222.5779
Nicole Werner, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Serena Chen, NYU Langone Health, New York, NY, United States; Abigail L. Nita, Indiana University School of Medicine, Fort Wayne, IN, United States; Olivia Lee, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Nikita Nagpal, New York University Grossman School of Medicine, New York, NY, United States; Carol Duh-Leong, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Stephanie Quintero Chacon, NYU Langone Health, East Elmhurst, NY, United States; Robin Ortiz, New York University Grossman School of Medicine, New York, NY, United States

Nicole Werner (she/her/hers)
Medical Student
Hassenfeld Children's Hospital at NYU Langone
New York, New York, United States
Presenting Author(s)
Background: Most children and adults in the U.S. do not meet nutrition guideline recommendations. Although collecting caregiver dietary history is not standard practice in pediatric visits, children’s dietary habits are significantly influenced by their caregivers’ and often reflect the dietary patterns of their households. Targeting the child-caregiver relationship in dietary interventions may foster healthier nutritional habits and related behaviors for the entire family.
Objective: To quantify average daily servings of fruits and vegetables in children and caregivers after implementation of a EHR prompt strategy in a public hospital primary care pediatric clinic.
Design/Methods: The EHR templates for well child visits in children aged 3-11 at a public hospital’s primary care pediatric clinic were updated to quantify the daily fruit and vegetable serving intake for the child and their caregiver.
Retrospective analysis of 600 charts was conducted over a 4-month period to quantify average intake in children and their caregivers.
A qualitative content analysis of dietary history was conducted, guided by the AAP’s healthy habits questionnaire, in a subset of charts to identify any mention of the caregiver’s or family’s dietary patterns.
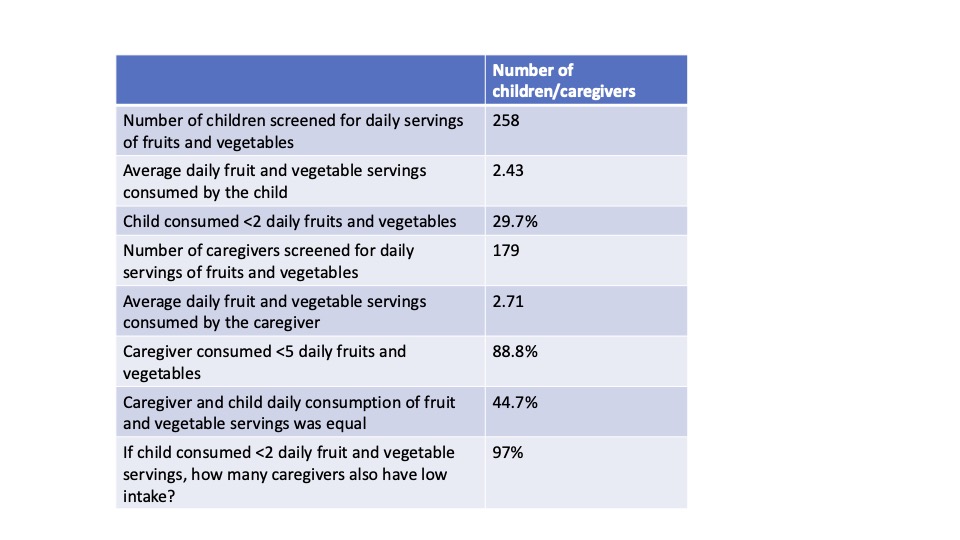
Results: After implementation of the updated EHR template, it was observed that 179 caregivers of children were screened for low fruit and vegetable intake, with 159 (88.8%) identified to have lower than recommended intake ( < 5 servings per day).
In visits that both the child and caregiver were screened, 44.7% had equivalent daily intake. Furthermore, when a child was found to have low fruit/vegetable intake, 97.1% of caregivers also had low intake. The Pearson’s correlation comparing the number of servings of fruit and vegetables in the child with that of the caregiver was 0.466 (r=0.47, p< 0.01).
Qualitative analysis found no documentation related to the caregiver’s diet (beyond fruit/vegetable intake) nor any documentation of family eating behaviors (such as the number of meals eaten together as a family each week) in any of the analyzed charts.
Conclusion(s): Our findings confirm that children in a public hospital system frequently fall short of recommended fruit and vegetable intake; notably, this finding can be effectively assessed in primary care by examining caregiver dietary patterns. Children’s fruit and vegetable consumption closely aligned with that of their caregiver’s, with particularly high concordance in cases of low intake. These results underscore the value of a family-centered approach to dietary counseling and intervention.
Table 1: Daily fruit and vegetable consumption among children and their caregivers