Neonatal Clinical Trials 1
Session: Neonatal Clinical Trials 1
559 - Three-year mortality and disability in very preterm and low birthweight infants cared for in single family rooms versus open bay units: Randomized Controlled Trial
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 559.6556
Michael J. Vincer, Dalhousie University Faculty of Medicine, Halifax, NS, Canada; Christy Woolcott, Dalhousie University Faculty of Medicine, Halifax, NS, Canada; Darlene J. Inglis, IWK HEALTH CENTRE, Bedford, NS, Canada; Tanya Myles, IWK Health, Halifax, NS, Canada; Susan MacDonald, Dalhousie University Faculty of Medicine, Bedford, NS, Canada; Jehier Afifi, Dalhousie University Faculty of Medicine, Halifax, NS, Canada; Charles "David" A. Simpson, Dalhousie University Faculty of Medicine, Halifax, NS, Canada; Satvinder ghotra, IWK Health Center, Halifax, NS, Canada; Walid El-Naggar, Dalhousie University Faculty of Medicine, Halifax, NS, Canada; Balpreet Singh, IWK Health Centre and Dalhousie University, Halifax, NS, Canada; Danielle Styranko, IWK Health Center, Halifax, NS, Canada; Sharon Unger, IWK Health Centre, Halifax, NS, Canada; Souvik Mitra, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Douglas D. McMillan, Dalhousie University, Calgary, AB, Canada; Jon Dorling, University Hospital of Southampton, Southampton, England, United Kingdom
.jpg)
Michael J. Vincer, MD (he/him/his)
Neonatologist (retired)
Dalhousie University Faculty of Medicine
Halifax, Nova Scotia, Canada
Presenting Author(s)
Background: Neonatal Intensive care units (NICU) are believed to be better with single family room (SFR) design compared to the more traditional open bay (OB) design. Nevertheless, mortality has been reported to be similar between SFR and OB and, in one study, SFR care was associated with lower language scores at two years of age in infants < 30 weeks’ gestational age.
Objective: Since no randomized controlled trials have examined the long-term outcome or the survival of high-risk infants, this trial was designed to compare these outcomes in SFR versus OB.
Design/Methods: Pre-Covid reconstruction of both level 3 NICUs at the Izaak Walton Killam Hospital, Halifax, Canada resulted in a 440-day period (11 April 2018 to 25 June 2019) in which one NICU was SFR and the other was OB. Infants admitted to NICU were randomly assigned to either SFR or OB using a computer generated algorithm weighted so that the less busy NICU was more likely to receive the next infant. Multiple births were allocated to the same Unit. Allocation was concealed; however, the study intervention could not be blinded. Very preterm ( < 31 weeks) and very low birthweight (VLBW < 1500 grams) infants, who were routinely enrolled in the long-term Perinatal Follow-Up Program, were eligible for the study. Infants were excluded if, a) they were admitted to NICU at more than 14 days of age, b) they had anomalies affecting survival or long-term development or c) they were admitted for palliative care only. The primary outcome was death or disability (language or cognitive delay on the Bayley Scales of Infant and Toddler Development (version IV), cerebral palsy, blindness or deafness) at three years corrected gestational age (CGA). Each component of the primary outcome was a secondary outcome.
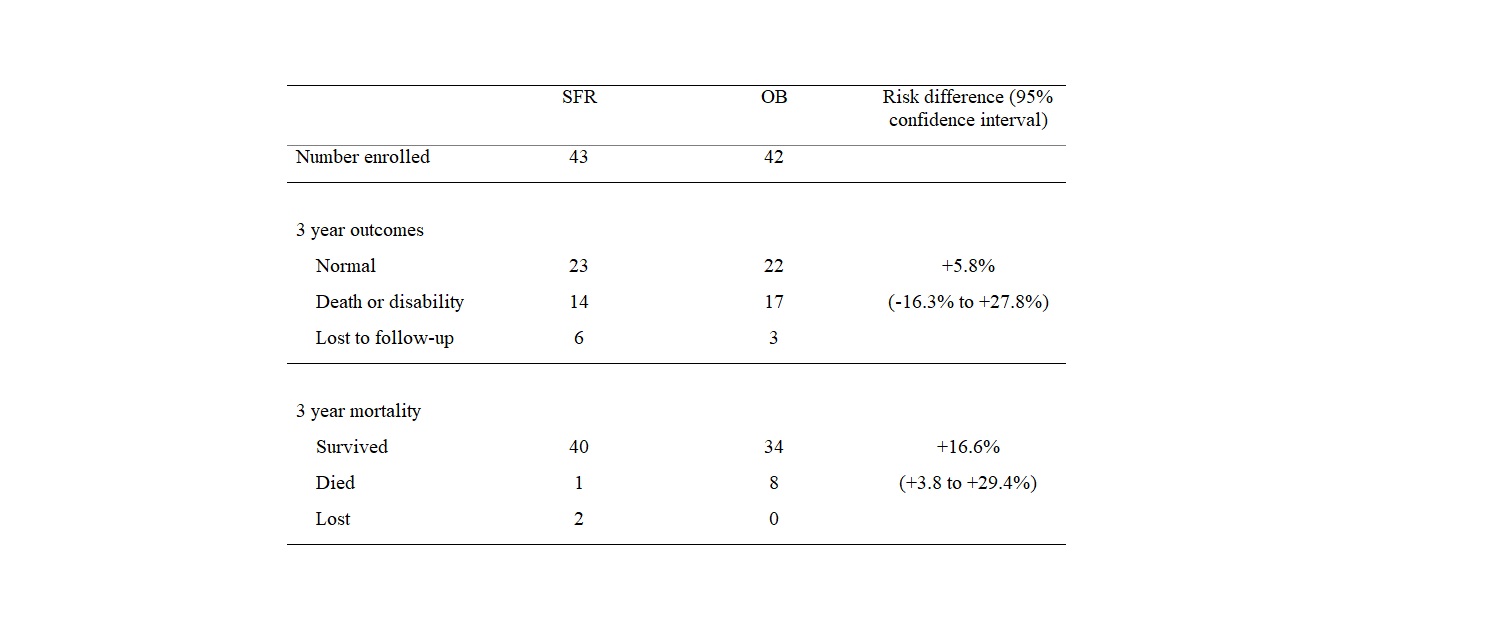
Results: 819 randomly allocated infants were admitted to NICU of which 85 were enrolled in the trial, 43 to SFR and 42 to OB (Figure). Initial state variables are noted in Table 1. The primary outcome did not differ between groups (Fisher exact p-value = 0.391); however, mortality (Table 2) was lower in SFR than OB (Fisher exact p-value = 0.029).
Conclusion(s): The disability rate was similar in the SFR compared to the OB NICU; however, there was a significant reduction in mortality in the SFR NICU.
Figure: Patient selection & enrollment
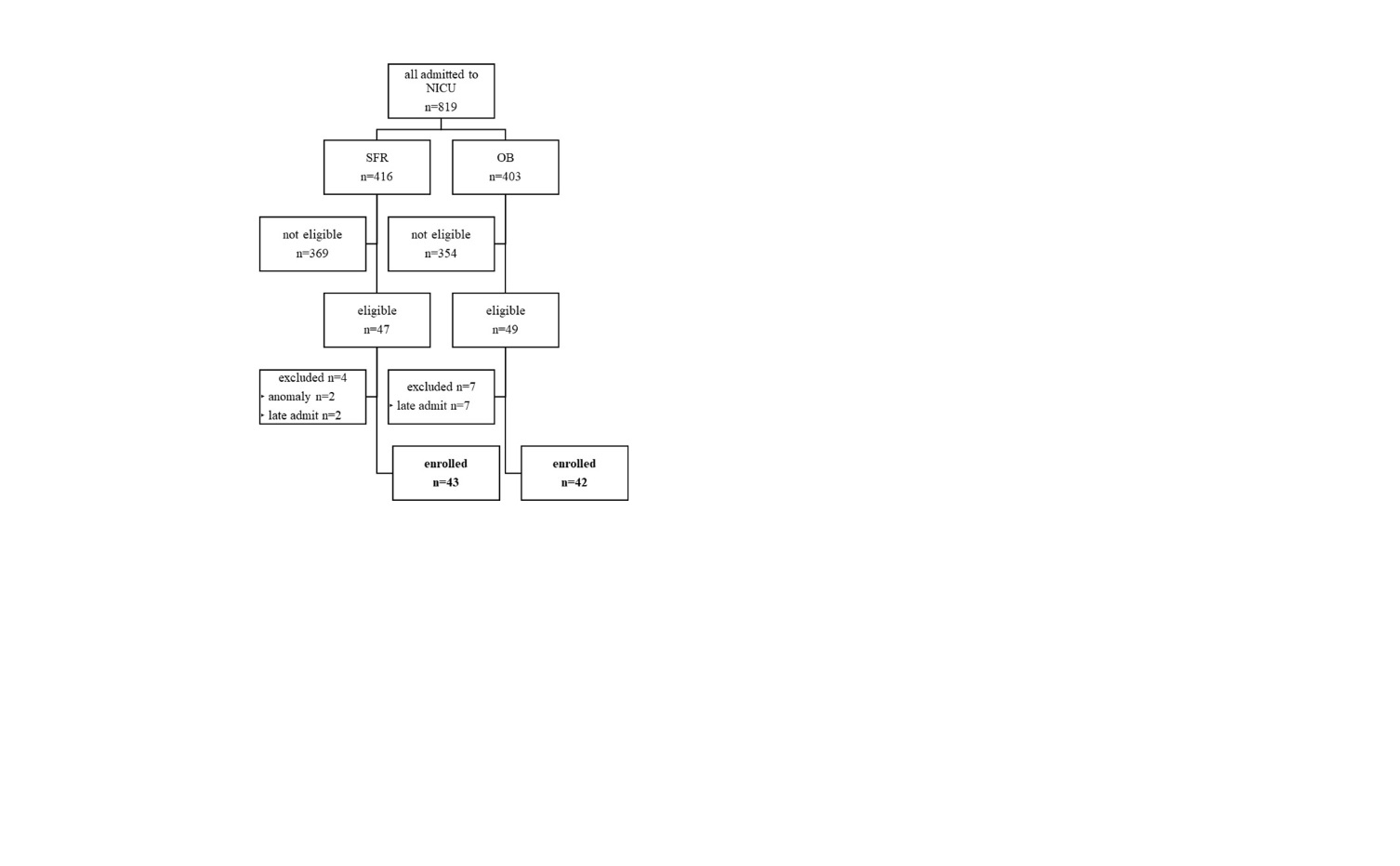
Table 1: Initial state variables
.jpg) * mean + standard error of the mean
* mean + standard error of the mean† number (%)
Table 2: Three year corrected gestational age outcomes
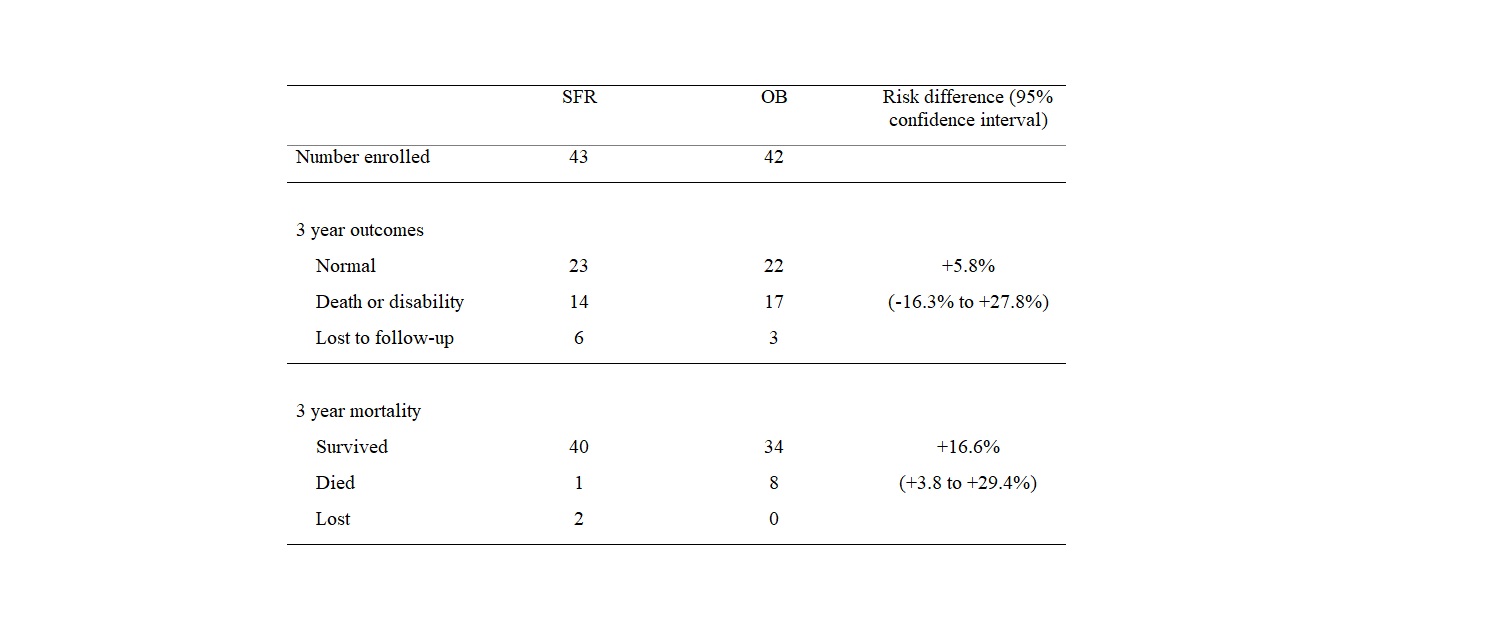
Figure: Patient selection & enrollment
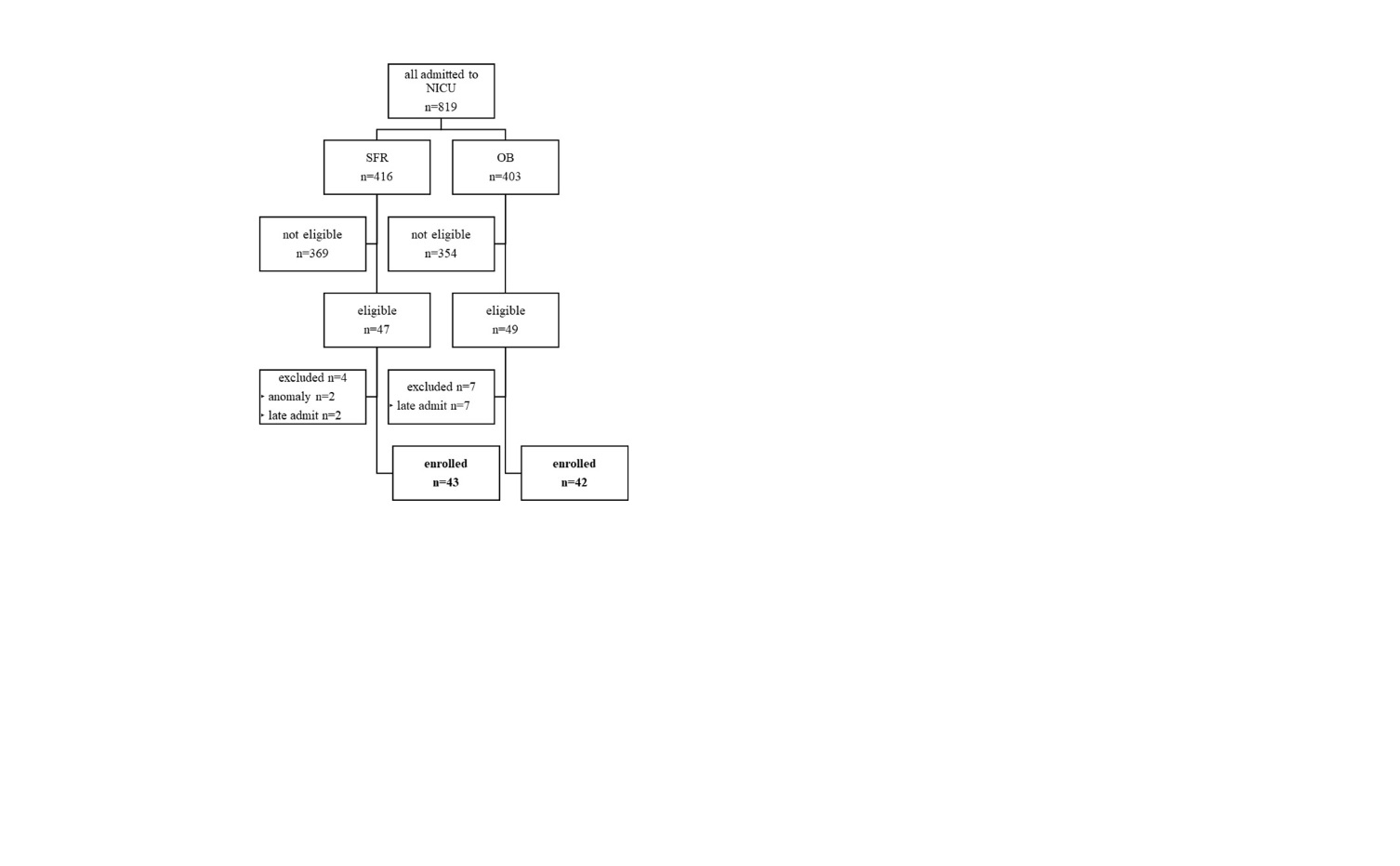
Table 1: Initial state variables
.jpg) * mean + standard error of the mean
* mean + standard error of the mean† number (%)
Table 2: Three year corrected gestational age outcomes