Environmental Health 1
Session: Environmental Health 1
440 - Associations of community material neighborhood deprivation with the diagnosis of asthma among children with bronchopulmonary dysplasia (BPD)
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 440.3607
Jonathan J. Szeto, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Joshua Radack, Childrens Hospital of Philadelphia, Boston, MA, United States; Sara B.. DeMauro, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Chen C. Kenyon, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Nicolas P. Goldstein Novick, Children's Hospital of Philadelphia, Rose Valley, PA, United States; Kristan Scott, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Daria Murosko, The Children's Hospital of Philadelphia, Philadelphia, PA, United States; Kathleen Gibbs, University of Pennsylvania/Children's Hospital of Philadelphia, Philadelphia, PA, United States; Nicolas Bamat, Childrens Hospital of Philadelphia, Swarthmore, PA, United States; Scott A. Lorch, The Children's Hospital of Philadelphia, Philadelphia, PA, United States; Paul E. Moore, Vanderbilt University School of Medicine, Btentwood, TN, United States; Heather H. Burris, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Timothy Nelin, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Timothy Nelin, MD (he/him/his)
Attending Physician
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Socioeconomic deprivation and BPD are known risk factors for asthma in children. Whether neighborhood socioeconomic factors increase asthma risk among children with BPD is unknown.
Objective: To quantify associations of the community-level material deprivation index (CMDI) with the diagnosis of asthma by age 5 among children diagnosed with BPD.
Design/Methods: We conducted a retrospective study of children diagnosed with BPD using the 2019 NRN criteria, born between 2010-2019, discharged from a single hospital system to a home address in the Philadelphia metropolitan area, with documented follow-up in the Children’s Hospital of Philadelphia Care Network. Patient charts were reviewed for a diagnosis of asthma by age 5, identified by ICD-9/10 code. We geocoded each patient’s address at time of NICU discharge to assign census tract CMDI values. The CMDI is composed of 6 variables (socioeconomic status variables and vacant housing) from the 2018 American Community Survey ranging from 0 to 1, with a higher score indicating higher deprivation. Multivariable logistic regression models quantified associations of CMDI with asthma by age 5 with robust variance estimates, adjusting for patient-level factors. Secondary analysis focused on asthma diagnosis among children discharged from the NICU without inhaled respiratory medications or supplemental support, as these factors may confound the causal pathway of asthma diagnosis in BPD. We did not consider race and ethnicity in modeling as these are socially constructed and not biologic or clinical factors.
Results: Of 346 children, 171 (49%) were diagnosed with asthma by age 5. Among infants diagnosed with asthma, CMDI was higher, birth weight and gestational age were lower, and a greater proportion were prescribed albuterol and inhaled corticosteroids (Table 1). Figure 1 displays regional variation in CMDI. Per standard deviation increment increase in CMDI, children had higher odds of an asthma diagnosis in models adjusted for infant sex, gestational age, birth weight, BPD grade, chronologic age at discharge, inhaled medication use and respiratory support at time of NICU discharge, year, and insurance type (aOR 1.29, 95%CI: 1.03-1.60). Results were similar when restricted to the 214 children without supplemental respiratory support or inhaled respiratory medication use at NICU discharge (aOR 1.40, 95% CI: 1.06-1.86).
Conclusion(s): Among children with BPD, higher neighborhood deprivation was associated with asthma diagnosis by age 5. Identifying place-based interventions to improve respiratory outcomes among former preterm infants with BPD should be a research priority.
Table 1. Bivariate associations of community material deprivation and patient characteristics with the asthma diagnosis by age 5 among preterm infants with bronchopulmonary dysplasia (BPD).
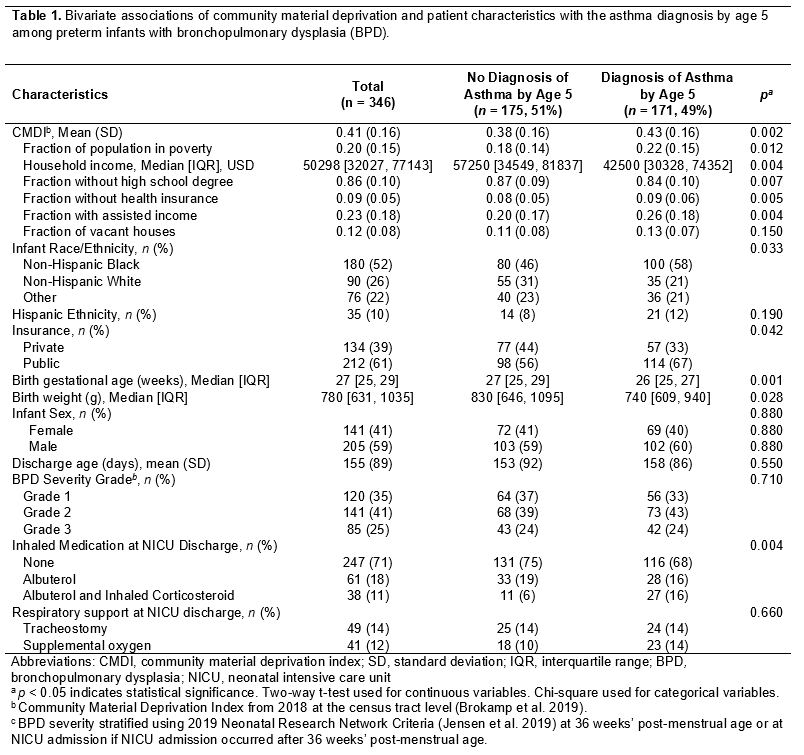
Figure 1.
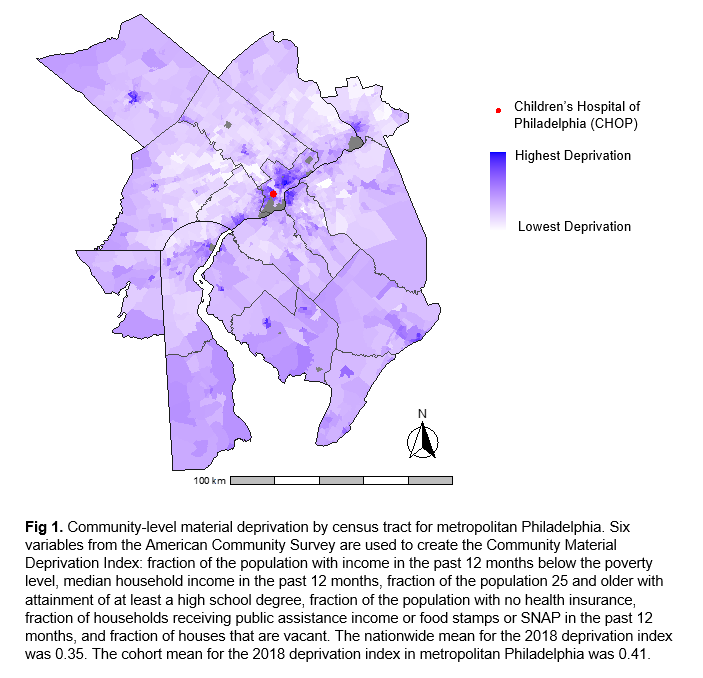 Community-level material deprivation by census tract for metropolitan Philadelphia. Six variables from the American Community Survey are used to create the Community Material Deprivation Index: fraction of the population with income in the past 12 months below the poverty level, median household income in the past 12 months, fraction of the population 25 and older with attainment of at least a high school degree, fraction of the population with no health insurance, fraction of households receiving public assistance income or food stamps or SNAP in the past 12 months, and fraction of houses that are vacant. The nationwide mean for the 2018 deprivation index was 0.35. The cohort mean for the 2018 deprivation index in metropolitan Philadelphia was 0.41.
Community-level material deprivation by census tract for metropolitan Philadelphia. Six variables from the American Community Survey are used to create the Community Material Deprivation Index: fraction of the population with income in the past 12 months below the poverty level, median household income in the past 12 months, fraction of the population 25 and older with attainment of at least a high school degree, fraction of the population with no health insurance, fraction of households receiving public assistance income or food stamps or SNAP in the past 12 months, and fraction of houses that are vacant. The nationwide mean for the 2018 deprivation index was 0.35. The cohort mean for the 2018 deprivation index in metropolitan Philadelphia was 0.41.Table 1. Bivariate associations of community material deprivation and patient characteristics with the asthma diagnosis by age 5 among preterm infants with bronchopulmonary dysplasia (BPD).
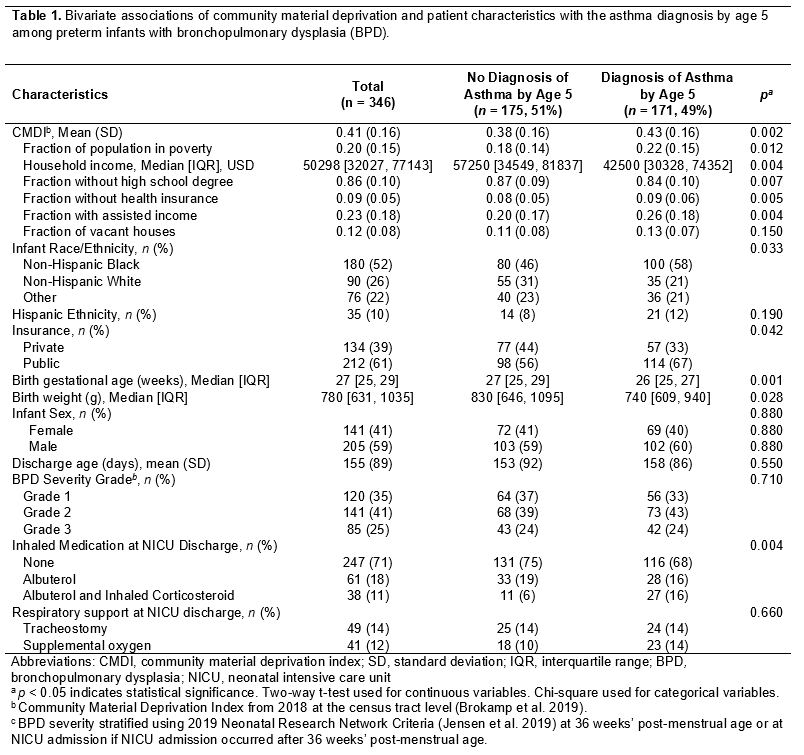
Figure 1.
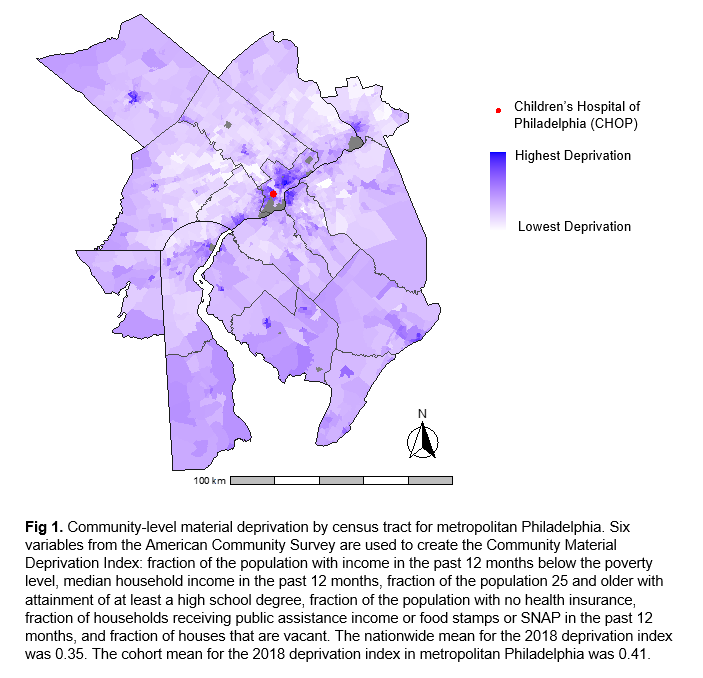 Community-level material deprivation by census tract for metropolitan Philadelphia. Six variables from the American Community Survey are used to create the Community Material Deprivation Index: fraction of the population with income in the past 12 months below the poverty level, median household income in the past 12 months, fraction of the population 25 and older with attainment of at least a high school degree, fraction of the population with no health insurance, fraction of households receiving public assistance income or food stamps or SNAP in the past 12 months, and fraction of houses that are vacant. The nationwide mean for the 2018 deprivation index was 0.35. The cohort mean for the 2018 deprivation index in metropolitan Philadelphia was 0.41.
Community-level material deprivation by census tract for metropolitan Philadelphia. Six variables from the American Community Survey are used to create the Community Material Deprivation Index: fraction of the population with income in the past 12 months below the poverty level, median household income in the past 12 months, fraction of the population 25 and older with attainment of at least a high school degree, fraction of the population with no health insurance, fraction of households receiving public assistance income or food stamps or SNAP in the past 12 months, and fraction of houses that are vacant. The nationwide mean for the 2018 deprivation index was 0.35. The cohort mean for the 2018 deprivation index in metropolitan Philadelphia was 0.41.
