Nephrology 6
Session: Nephrology 6
631 - Evaluating Trends in End-Stage Renal Disease Secondary to Reflux Nephropathy
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 631.4591
Alexander J. Wolf, Lucile Packard Children's Hospital Stanford, San Francisco, CA, United States; Sai liu, Stanford University School of Medicine, palo alto, CA, United States; Margaret R. Stedman, Stanford University, Palo Alto, CA, United States; Paul Grimm, Stanford University, Medical S, Palo Alto, CA, United States; Abanti Chaudhuri, Stanford University, Stanford, CA, United States; David Hains, Indiana University School of Medicine, Indianapolis, IN, United States; Michelle Starr, Indiana University School of Medicine, Indianapolis, IN, United States; Kathleen M. Kan, Stanford University School of Medicine, San Bruno, CA, United States; Scott Sutherland, Stanford University School of Medicine, Palo Alto, CA, United States; Alan Schroeder, Stanford University School of Medicine, Palo Alto, CA, United States

Alexander J. Wolf, MD (he/him/his)
Fellow, Pediatric Nephrology
Lucile Packard Children's Hospital Stanford
San Francisco, California, United States
Presenting Author(s)
Background: Up to 50% of children with urinary tract infections (UTIs) have vesicoureteral reflux (VUR). Severe VUR can lead to reflux nephropathy (RN) and end-stage renal disease (ESRD). VUR is diagnosed by voiding cystourethrogram (VCUG). While the 1999 AAP UTI guidelines recommended VCUGs for all first-UTIs, the 2011 guidelines suggest VCUGs only for patients with recurrent UTIs or ultrasound abnormalities. Consequently, VCUGs have decreased. There is continued debate whether delayed or missed diagnoses of VUR, and the resultant reduction in therapeutic interventions, may be causing preventable renal damage.
Objective: To evaluate recent trends in the US incidence of pediatric ESRD overall and specifically in ESRD attributed to RN. Also, due to a history of race-based medicine within UTI management, to identify potential socioeconomic and racial disparities for these diagnoses.
Design/Methods: We conducted a retrospective cohort study using the United States Renal Data System (USRDS), a database that includes 100% of US patients treated for ESRD each with an assigned ICD code for primary cause of ESRD. We identified patients aged 0-24 years with ESRD attributed to RN from 2002-2021, as well as related etiologies including dysplasia and obstructive uropathies. We used US Census Bureau data to ascertain population incidence and a Poisson regression model for incidence rate ratios (IRR). We collected demographic information to compare the RN cohort to all ESRD patients.
Results: Demographic data for the 43,158 patients aged 0-24 with incident ESRD between 2002-2021 are summarized in Table 1. There were 1,026 (2.4%) ESRD cases attributed to RN. While Black patients are overrepresented for overall ESRD (11,815 patients, or 27.4%), they are underrepresented in RN (80 patients, or 7.8%). The all-cause incidence of ESRD has decreased (IRR of 0.987 per year, p< 0.001), as did ESRD due to RN (IRR of 0.951 per year, p< 0.001). ESRD from etiologies related to RN decreased slightly. Incidence data are plotted in Figures 1 and 2.
Conclusion(s): We found no evidence that the incidence of pediatric ESRD due to RN has increased over our study period. These findings provide some reassurance that renal outcomes have not worsened with decreased VCUG use. However, the reduced incidence of RN may reflect an underdiagnosis of VUR (and thus future RN) in the absence of a VCUG. Continued surveillance over time and investigations into shorter-term renal outcomes are needed. Further study is also needed to assess the root cause of racial disparities in the RN cohort and the possibility that Black children with VUR are going undiagnosed.
Wolf Confirmation of Training Status.pdf
Figure 1.
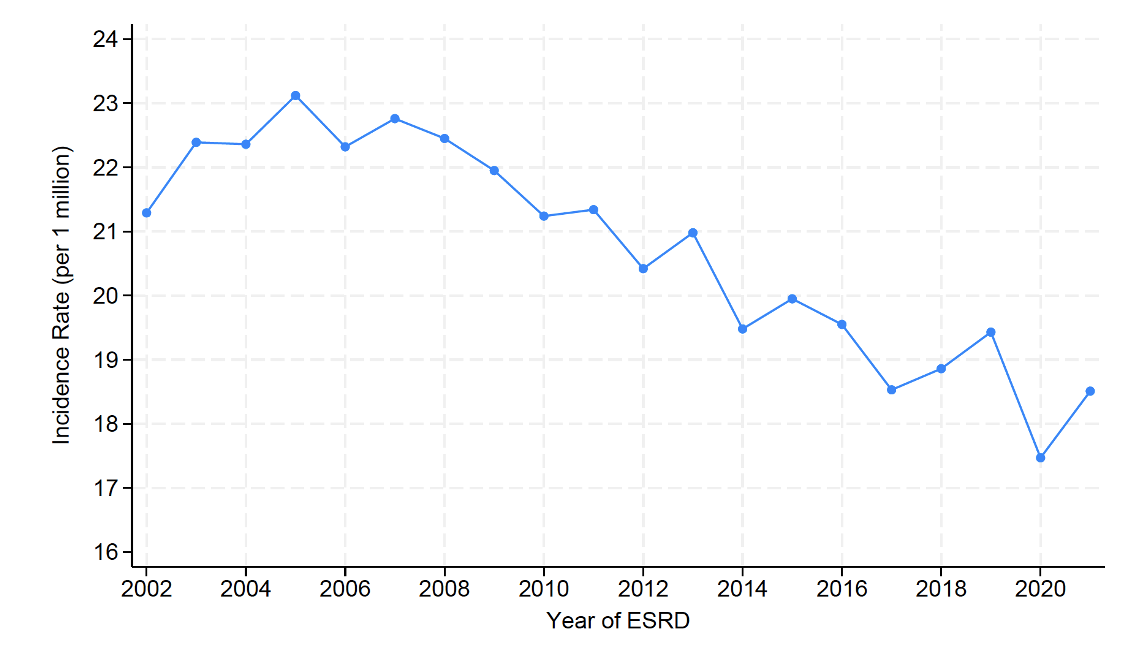 Incidence of ESRD from 2002-2021 in patients aged 0-24 by all causes.
Incidence of ESRD from 2002-2021 in patients aged 0-24 by all causes.Figure 2.
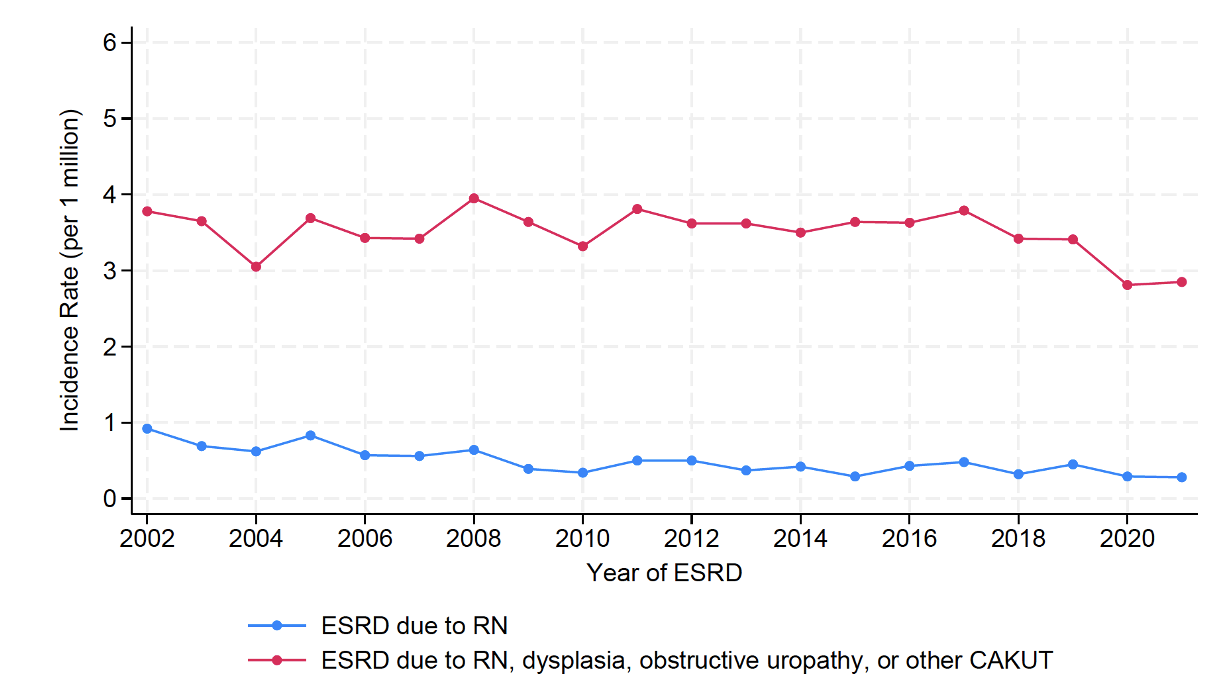 Incidence of ESRD from 2002-2021 in patients aged 0-24 due to reflux nephropathy and combined reflux nephropathy with overlapping diagnoses (dysplasia, obstructive uropathies, and other CAKUTs).
Incidence of ESRD from 2002-2021 in patients aged 0-24 due to reflux nephropathy and combined reflux nephropathy with overlapping diagnoses (dysplasia, obstructive uropathies, and other CAKUTs).Wolf Confirmation of Training Status.pdf
Figure 1.
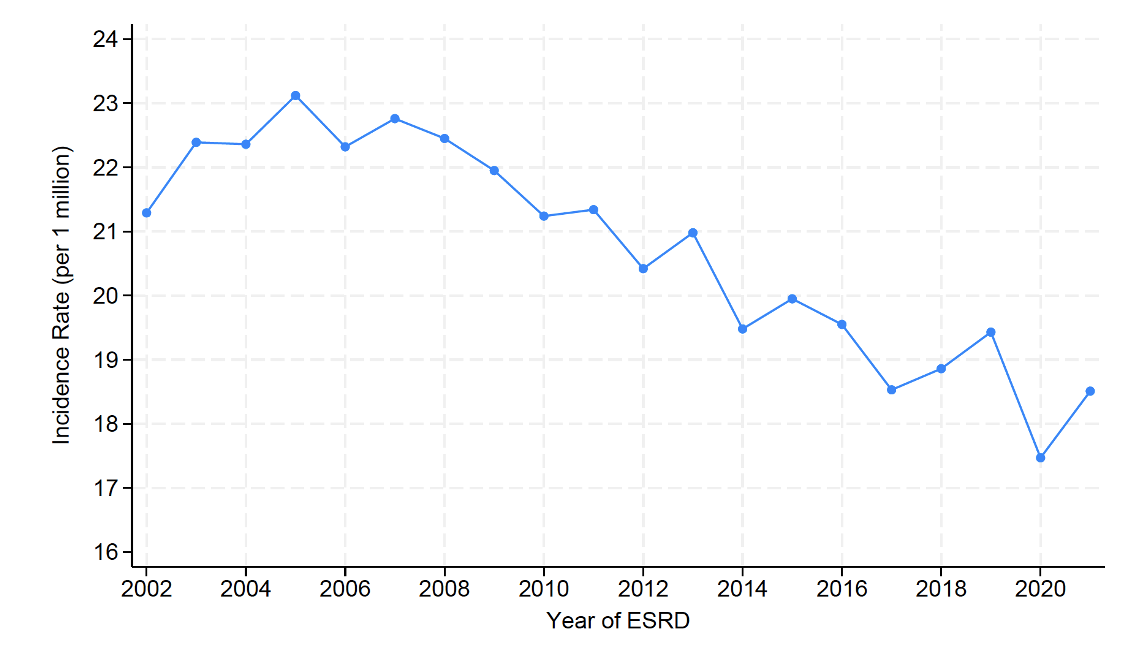 Incidence of ESRD from 2002-2021 in patients aged 0-24 by all causes.
Incidence of ESRD from 2002-2021 in patients aged 0-24 by all causes.Figure 2.
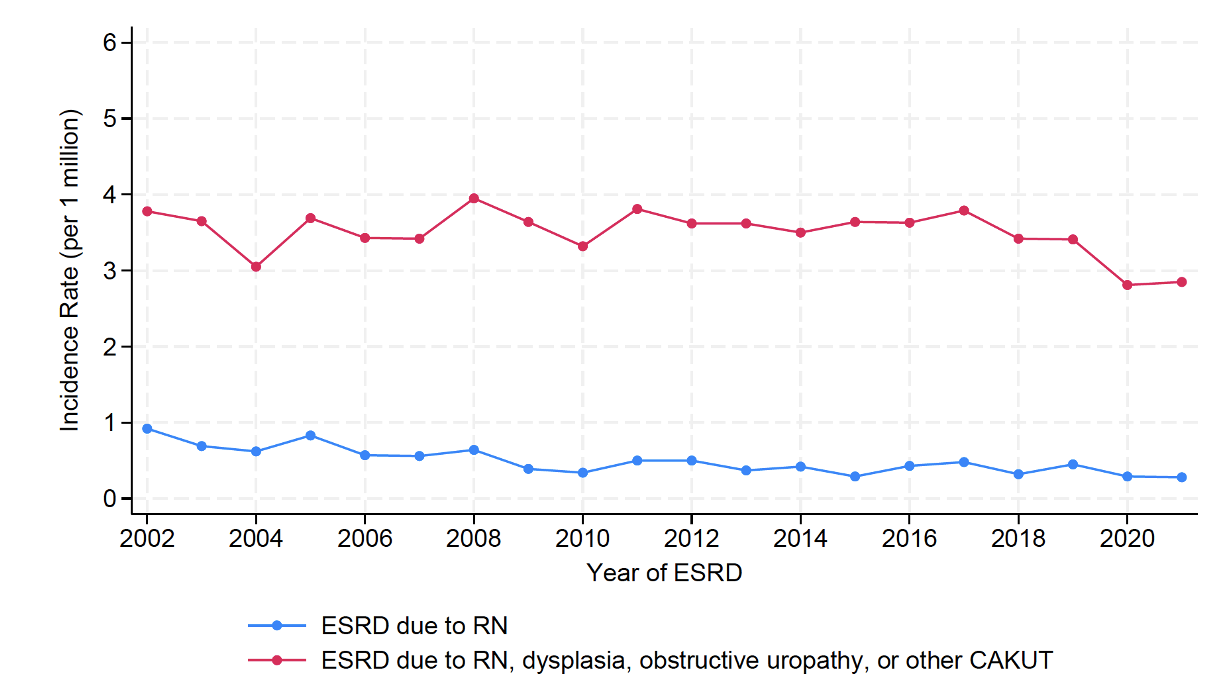 Incidence of ESRD from 2002-2021 in patients aged 0-24 due to reflux nephropathy and combined reflux nephropathy with overlapping diagnoses (dysplasia, obstructive uropathies, and other CAKUTs).
Incidence of ESRD from 2002-2021 in patients aged 0-24 due to reflux nephropathy and combined reflux nephropathy with overlapping diagnoses (dysplasia, obstructive uropathies, and other CAKUTs).
