Historical Perspectives
Session: Historical Perspectives
811 - Moments of Transition: The Journey of Umbilical Cord Clamping Practices
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 811.5823
Suleiman Essoh, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Muppala Prasanth Raju, Baylor Scott White McLane Children's Medical Center, Temple, TX, United States; Niraj Vora, Baylor Scott White McLane Children's Medical Center, LEANDER, TX, United States; Venkata N. Raju, Baylor Scott & White Hospitals, Coppell, TX, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States; Anup Katheria, Sharp Mary Birch Hospital for Women & Newborns, San Diego, CA, United States

Niraj Vora, MD, FAAP
Division Chief and Fellowship Program Director, Assistant Professor of Pediatrics
Baylor Scott White McLane Children's Medical Center
LEANDER, Texas, United States
Presenting Author(s)
Background: Umbilical cord clamping practices have changed significantly over centuries, moving from a traditional formality to an evidence-based practice. Early cord clamping (ECC) intruded into clinical practice in the late 19th century, despite evidence demonstrating that a placental transfusion offered benefits.
Objective: To trace the evolution of cord-clamping practices.
Design/Methods: Historical records, clinical guidelines, observational studies, randomized controlled trials, and meta-analysis were reviewed.
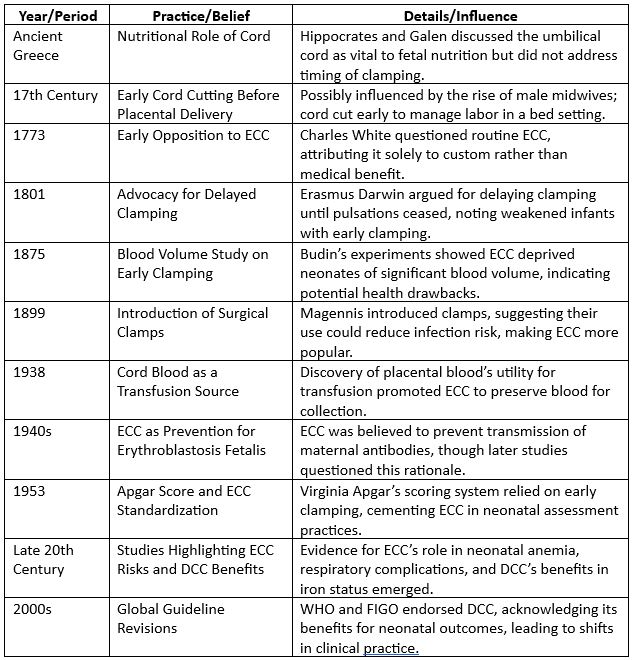
Results: Eleven practices were identified (table 1) with varied definitions of early and late clamping. There were 12 individuals or committee guidelines that had a large influence on cord clamping practices. Hippocrates and Galen acknowledged the umbilical cord’s role in fetal health without focusing on clamping timing. Ayurvedic medicine believes that delaying cord clamping enhances the overall health and vitality of the newborn. By 18th century, Erasmus Darwin recommended waiting for pulsations to stop to avoid weakening newborns. The 19th and 20th centuries saw ECC take root, largely due to new surgical clamps and early theories suggesting ECC might prevent erythroblastosis fetalis. Rh(D) Immune Globulin later diminished the relevance of ECC. Additionally, Apgar score, introduced in 1953, and fear of cerebral palsy encouraged ECC. ECC also became a norm with growing hospital deliveries and caesarian sections with obstetricians taking over from midwives.
This shift in ECC to DCC was influenced by studies by Yao et al- on increased blood volume and iron stores and a decrease in anemia incidence in DCC infants. More recently Robledo et al and Anderson et al studied the neurodevelopmental outcomes in infants with favored DCC. DCC was further strengthened by studies reporting reduced in-hospital mortality by Tarnow-Mordi et al in preterm infants.
Growing evidence now highlights the benefits of allowing more time before clamping leading to improved neonatal outcomes with better iron levels and oxygenation in infants. Organizations such as WHO, FIGO, AAP, and ACOG endorse delayed cord clamping (DCC). All the recent trials demonstrate improved survival in preterm infants and better neurodevelopmental outcomes in term infants. "Delayed" clamping might simply represent a return to physiological norms rather than an actual delay. This shift is a reminder that neonatal care is a blend of tradition, advancing science, and individualized patient care.
Conclusion(s): The transition from ECC to DCC underscores neonatal care’s evolution toward evidence-based practices.
Evolution of different practices of Cord Clamping
Clinical Trials and Meta-analysis on Cord Clamping and significant contributors
.jpg)
Infograph on Umbilical Cord Clamping practice evolution
.jpg)

