Neonatal Clinical Trials 1
Session: Neonatal Clinical Trials 1
563 - Respiratory Morbidity in Extremely Preterm Infants Randomized to Receive either Early or Delayed Human Milk Fortification: A Secondary Analysis
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 563.6391
Marley J. Tucker, University of Alabama at Birmingham, Birmingham, AL, United States; Seabrook Jeffcoat, University of Alabama at Birmingham, Birmingham, AL, United States; Tori Argent, University of Alabama School of Medicine, Birmingham, AL, United States; Ariel A.. Salas, University of Alabama School of Medicine, Birmingham, AL, United States
Ariel A. Salas, MD, MSPH
Associate Professor
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Observational data suggest that providing higher energy intake to critically ill infants during the first week after birth is associated with a lower risk of bronchopulmonary dysplasia (BPD).
Objective: This secondary analysis of a masked randomized clinical trial aims to determine whether infants randomized to receive higher energy intake through early human milk fortification have a lower risk of BPD at 36 weeks of postmenstrual age (PMA).
Design/Methods: This is a post-hoc, secondary analysis of the IMPACT trial (NCT04325308) in which infants born at 28 weeks of gestation or less were randomized to receive fortified human milk at either postnatal day 3 or postnatal day 14. Daily fluctuations in weight, fluid intake, and serum sodium values were assessed using unadjusted repeated measures mixed models. Weight measurements were converted into z-scores using the INTERGROWTH-21st growth curves. A human milk sample was collected between postnatal day 7 and 10 and analyzed for macronutrient content to assess differences in energy and protein intake between groups. The BPD Jensen criteria were used to define respiratory morbidity at 36 weeks PMA.
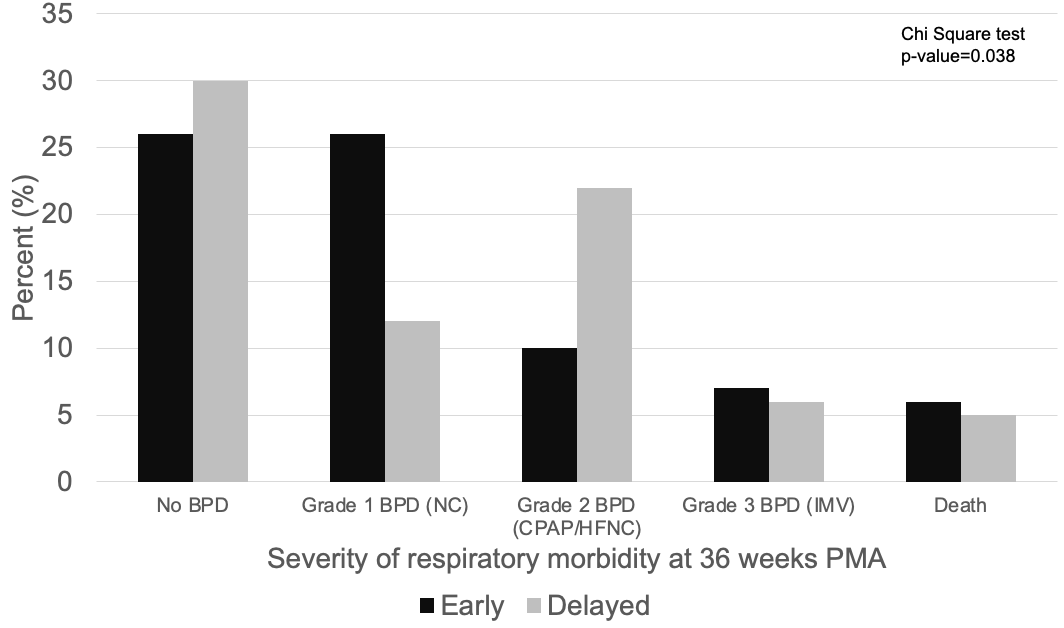
Results: Respiratory outcomes of 150 extremely preterm infants were analyzed (median gestational age: 26 weeks; mean birthweight: 750 g). Total fluid intake and enteral fluid intake did not differ between groups, but cumulative weight loss expressed in percentages (Fig 1A) and declines in weight-for-age z scores (Fig 1B) was more excessive in the delayed fortification group. The macronutrient analysis of 101 human milk samples revealed that early human milk fortification resulted in higher energy intake (median difference: +10kcal/100 ml; 95% CI: 3 to 15 kcal/100 ml; p=0.0001) and higher true protein intake (median difference: +0.4g/100 ml; 95% CI: 0.1 to 0.7g/100 ml; p=0.002), but not higher protein/energy ratios (median difference: +0.3g/100 kcal; 95% CI: -0.1 to 0.7 g/100 kcal; p=0.19), The severity of respiratory morbidity at 36 weeks PMA differed between groups (Figure 2). Although the proportions of survival without BPD and severe BPD at 36 weeks PMA were similar between groups, moderate BPD occurred more frequently in the delayed fortification group (p=0.038).
Conclusion(s): Early human milk fortification, through the provision of higher energy intake during the first two weeks after birth, may be associated with a lower severity of respiratory morbidity in critically ill infants born extremely preterm.
Figure 1. Longitudinal variation in the percentage of weight loss (A) and declines in weight-for-age z scores (B) in infants born extremely preterm.
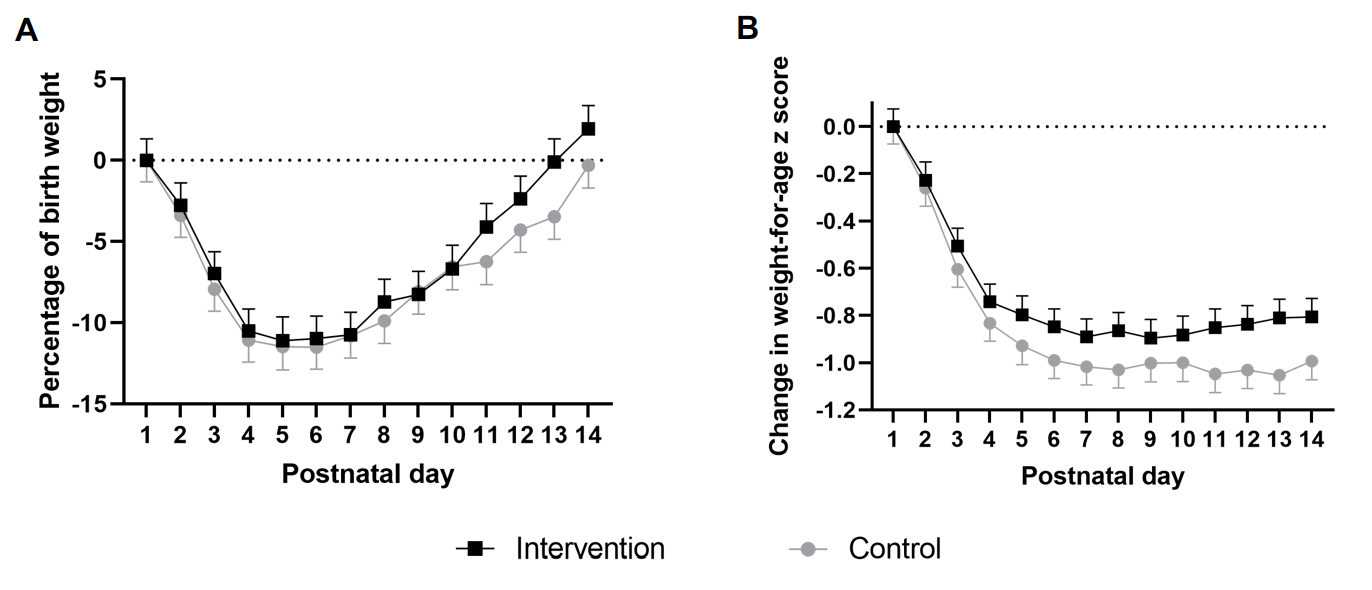
Figure 2. Respiratory morbidity at 36 weeks PMA in infants randomized to receive either early or delayed human milk fortification.