Neonatal Neurology 5: Fetal
Session: Neonatal Neurology 5: Fetal
673 - Placental Effects on Early Postnatal Cerebral Autoregulation in Neonates with Hypoplastic Left Heart Syndrome
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 673.6413
Ritu R. Trivedi, University of Texas Southwestern Medical School, Dallas, TX, United States; Marjorie Navalta, The University of Texas Southwestern, Dallas, TX, United States; Molly McGetrick, The University of Texas Southwestern Medical Center, Dallas, TX, United States; Rachel L.. Leon, University of Texas Southwestern Medical School, Dallas, TX, United States
Marjorie Navalta, BSN, RN (she/her/hers)
Research Nurse
The University of Texas Southwestern
Dallas, Texas, United States
Presenting Author(s)
Background: Neonates with severe forms of congenital heart disease (CHD) such as hypoplastic left heart syndrome (HLHS) are at increased risk of delayed brain development and brain injury. Disorders of the placenta have been linked to brain abnormalities in this population, but mechanisms by which the placenta increases this risk are unknown. We hypothesize that placental pathologies impact the development of cerebral autoregulation (CAR), leading to higher risk of brain injury and delayed brain development. Placental vascular malperfusion lesions may be most likely to exert deleterious effects on cerebral hemodynamics.
Objective: In neonates with HLHS, we compared the percentage of time spent with impaired CAR during the early postnatal period in those with normal healthy placenta versus those with histopathologic lesions of the placenta.
Design/Methods: In this single center observational cohort study, we analyzed time synchronized vital sign data in neonates with HLHS born at ³35 weeks gestation. CAR was determined in the early postnatal and pre-operative time period using the temporal relationship between mean arterial blood pressure (MAP) and regional cerebral oxygen saturation (rSO2). To assess intact versus impaired CAR, we used a rolling calculation of the Cerebral Oximetry Index (COx), a dynamic correlation in which values >0.3 were considered impaired CAR in accordance with prior studies. Placental pathologic diagnoses were made using Amsterdam guidelines. We used student t-test to determine differences between mean time spent with impaired CAR in HLHS neonates with normal versus abnormal placentas. In subgroup analyses, we compared those with normal placentas to neonates with vascular malperfusion lesions of the placenta.
Results: In our cohort of 26 neonates with HLHS, we analyzed an average of 86 hours of continuous monitoring (range 18-153). There were a total of 18 (69%) patients with evidence of placental pathology and 8 (31%) with normal placentas. COx showed a wide range in time spent with impaired CAR between subjects (range 0-35%, Fig 1). Mean time spent with impaired CAR in those with normal placentas was significantly less than those with placental histopathology (3.0 ± 1.8% vs. 8.4 ± 9.0%; p=0.02, Fig 2). In exploratory subgroup analysis, those with vascular malperfusion lesions of the placenta had similar time spent with impaired CAR (8.8 ± 6.5%; n=5) to those with normal placentas (p=0.12).
Conclusion(s): In neonates with severe forms of CHD such as HLHS, placental histopathologies may increase the risk of brain injury through disrupted development of cerebral autoregulation.
Early Postnatal Cerebral Autoregulation in Neonates with Hypoplastic Left Heart Syndrome (HLHS)
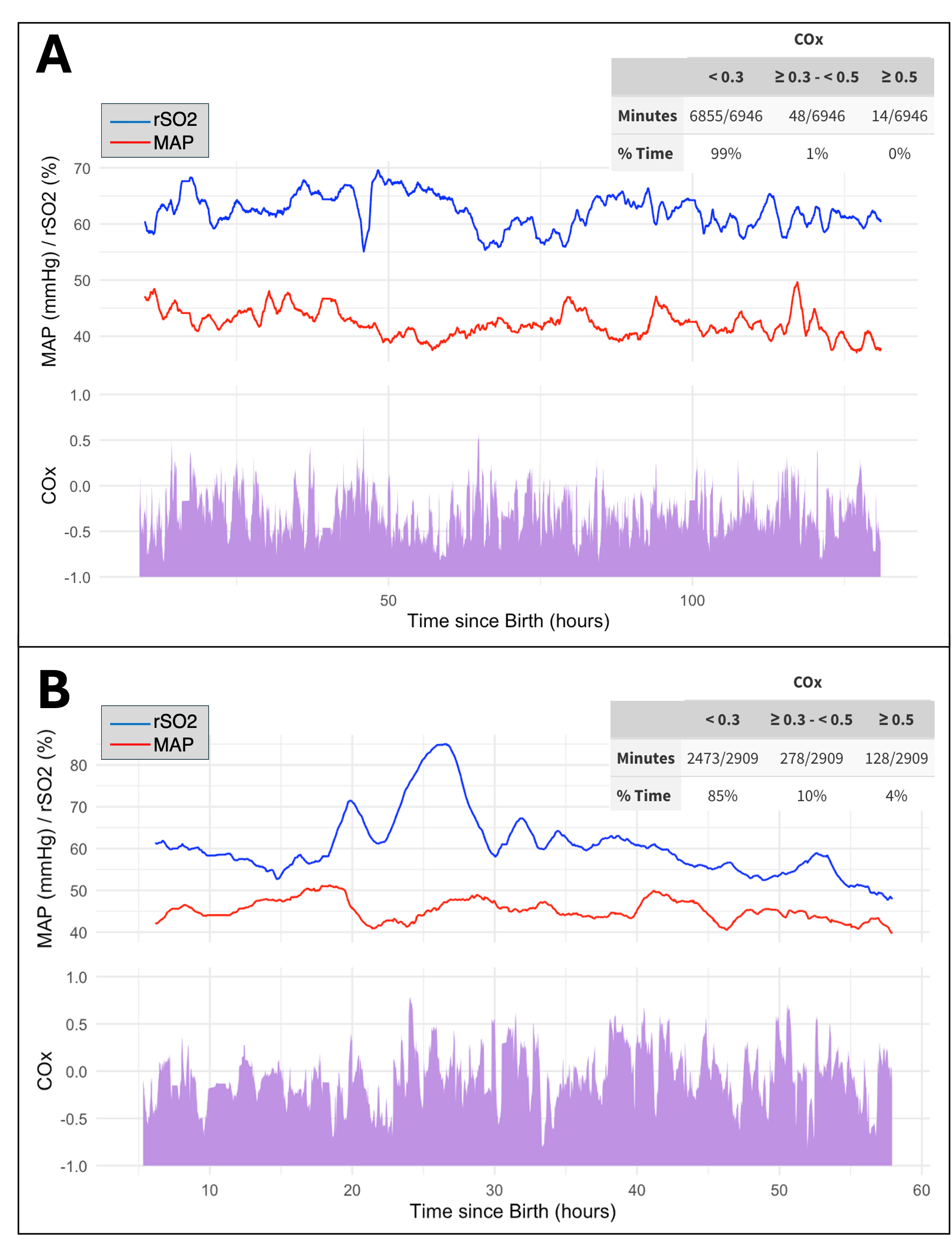 Example tracings of mean arterial pressure (MAP) and cerebral regional oxygen saturation (rSO2) in the early postnatal period along with time synchronized cerebral autoregulation (CAR) as measured by the cerebral oximetry index (COx). Example of neonate with intact CAR (A) and neonate with impaired CAR (B). Inset table of COx values shows minutes spent with COx in normal ( <0.3), slightly abnormal (>0.3 to <0.5) and abnormal (>0.5) ranges.
Example tracings of mean arterial pressure (MAP) and cerebral regional oxygen saturation (rSO2) in the early postnatal period along with time synchronized cerebral autoregulation (CAR) as measured by the cerebral oximetry index (COx). Example of neonate with intact CAR (A) and neonate with impaired CAR (B). Inset table of COx values shows minutes spent with COx in normal ( <0.3), slightly abnormal (>0.3 to <0.5) and abnormal (>0.5) ranges.Placental Pathology and Time Spent with Impaired Cerebral Autoregulation (CAR)
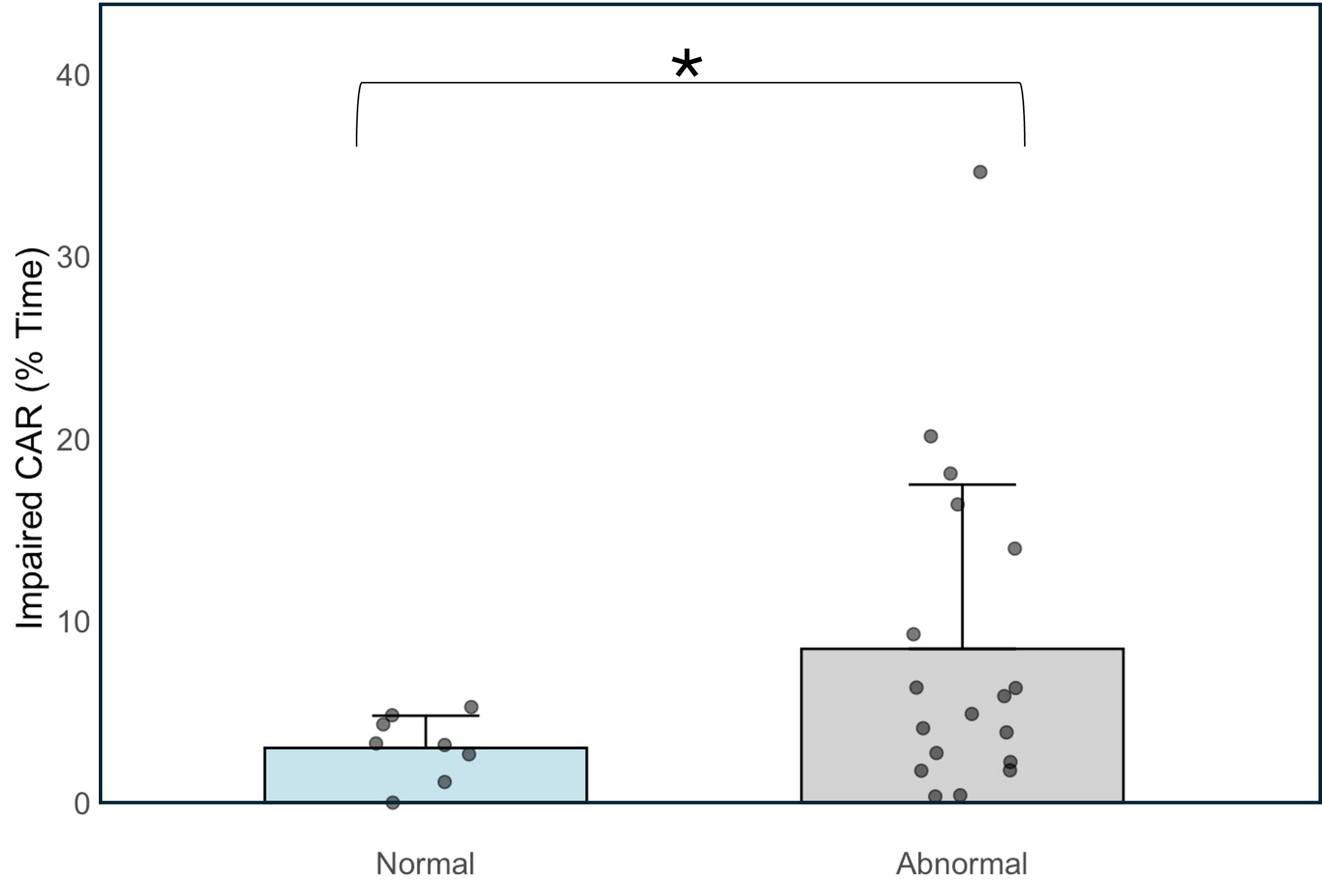 Mean percentage of time spent with impaired CAR in neonates with hypoplastic left heart syndrome (HLHS) and normal placenta (3.0 ± 1.8%; n=8) compared to those with histopathologic abnormalities of the placenta (8.4 ± 9.0%; n=18). *p < 0.05
Mean percentage of time spent with impaired CAR in neonates with hypoplastic left heart syndrome (HLHS) and normal placenta (3.0 ± 1.8%; n=8) compared to those with histopathologic abnormalities of the placenta (8.4 ± 9.0%; n=18). *p < 0.05
