Environmental Health 1
Session: Environmental Health 1
442 - Epidemiologic Trends in Pediatric Lead Poisoning at Freestanding Children's Hospitals (2016-2023)
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 442.4643
Phillip D.. Hahn, Boston Children's Hospital, Boston, MA, United States; Carly E.. Milliren, Boston Children's Hospital, Boston, MA, United States; Dionne A. Graham, Boston Children's Hospital, Boston, MA, United States; Diane Story, Boston Children's Hospital, Boston, MA, United States; Marissa Hauptman, Boston Children's Hospital, Boston, MA, United States
.jpg)
Marissa Hauptman, MD, MPH (she/her/hers)
Co-Director
Pediatric Environmental Health Center, Boston Children’s Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Severe childhood lead poisoning remains a critical public health challenge, with long-lasting effects on cognitive development, particularly in underserved communities disproportionately exposed to environmental toxins.
Objective: This study aimed to describe the epidemiology of inpatient and emergency department (ED) encounters for pediatric lead poisoning at US freestanding children’s hospitals.
Design/Methods: This retrospective cohort study used data from the Pediatric Hospital Information System from 2016–2023 and included encounters for patients with a primary diagnosis of lead poisoning who were ≤18 years of age at admission. Descriptive statistics were used to describe patient sociodemographic factors, clinical characteristics, and ED and hospital utilization. Poisson regression accounting for hospital state-level variation using generalized estimating equations was used to estimate and compare the rate of lead poisoning by patient sociodemographic factors, including race and ethnicity, insurance payor, urban status, and childhood opportunity index (COI) level.
Results: There were 1,982 encounters for lead poisoning across 47 PHIS hospitals; 845 inpatient hospitalizations, 1,137 ED visits. The majority were patients 1-3 years of age (68.4%) with public insurance (81.1%) residing in an urban ZIP code (92.2%) classified as very low or low COI (71.7%) with median household income less than $40,000 (71.9%) (Table 1). Iron deficiency was the most frequent comorbid diagnosis (inpatient: 41.4%, ED: 2.9%). Mean billed charges per case were $40,817 (SD=$62,477) and the mean cumulative annual billed charges was $4.31 million (SD=$915,546) (Figure 1). In adjusted models, patients who identified as Asian, non-Hispanic, Black, non-Hispanic, and multiracial, non-Hispanic had significantly higher rates of encounters for lead poisoning compared to White, non-Hispanic patients (Figure 2). Patients with public insurance had significantly higher rates of encounters than those with commercial (Figure 2) and those in rural ZIP codes had higher rates than urban (Figure 2). Patients in low and very low COI ZIP codes had significantly higher rates of encounters compared to patients in very high COI ZIP codes (Figure 2).
Conclusion(s): This study highlights the persistence of healthcare utilization and the economic burden of pediatric lead poisoning on healthcare systems. We found significant environmental inequities in the rate of hospitalization and emergency department utilization for lead poisoning by patient sociodemographic factors that warrant strengthened primary and secondary prevention initiatives.
Table 1
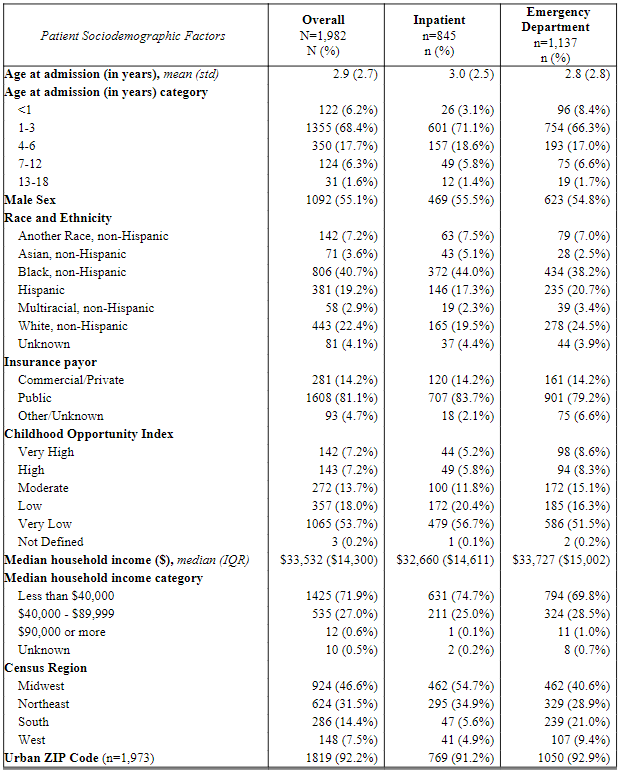 Patient sociodemographic factors among patients with encounters for lead poisoning by encounter type (N=1,982).
Patient sociodemographic factors among patients with encounters for lead poisoning by encounter type (N=1,982). Figure 1
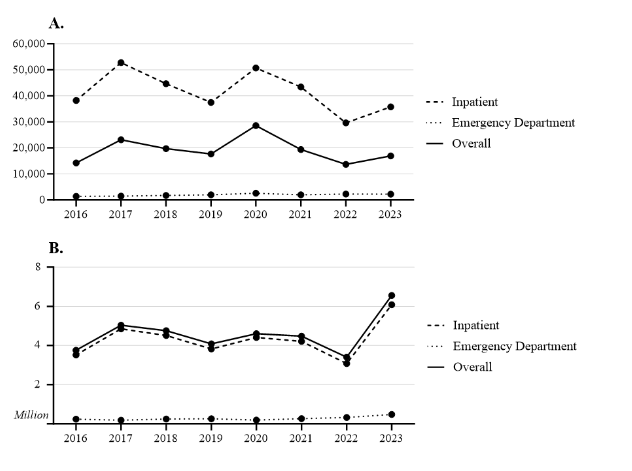 A) Mean total billed charges ($) and B) cumulative total billed charges ($, millions) for patients with lead poisoning by year and encounter type (n=1,982).
A) Mean total billed charges ($) and B) cumulative total billed charges ($, millions) for patients with lead poisoning by year and encounter type (n=1,982). Figure 2
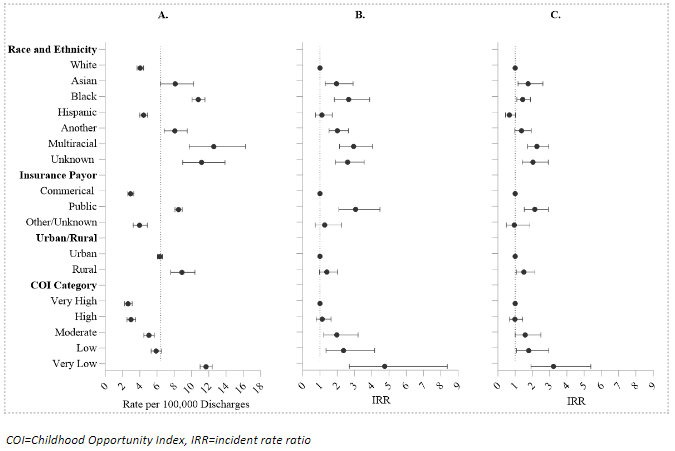 A) Crude rate of encounters for lead poisoning by patient sociodemographic factors, B) unadjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, and C) adjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, inpatient and emergency department, 2016-2023 (n=1,982).
A) Crude rate of encounters for lead poisoning by patient sociodemographic factors, B) unadjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, and C) adjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, inpatient and emergency department, 2016-2023 (n=1,982).Table 1
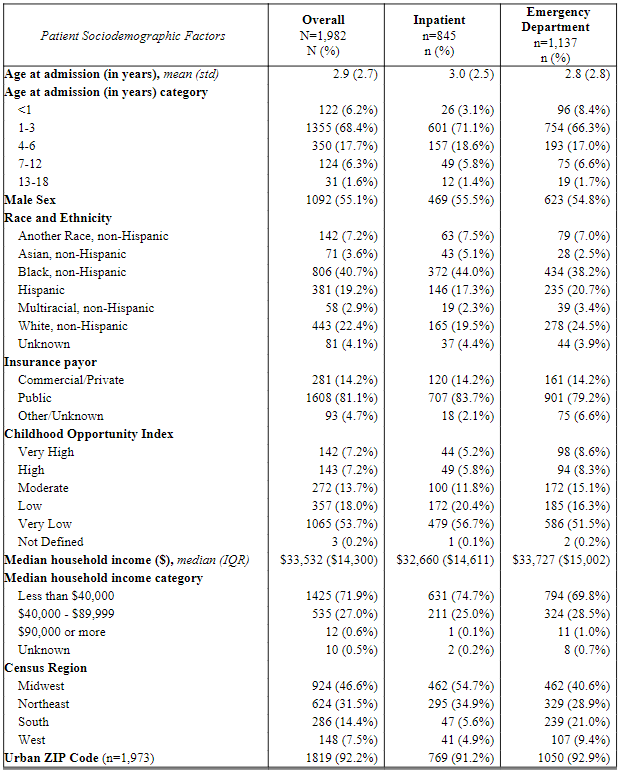 Patient sociodemographic factors among patients with encounters for lead poisoning by encounter type (N=1,982).
Patient sociodemographic factors among patients with encounters for lead poisoning by encounter type (N=1,982). Figure 1
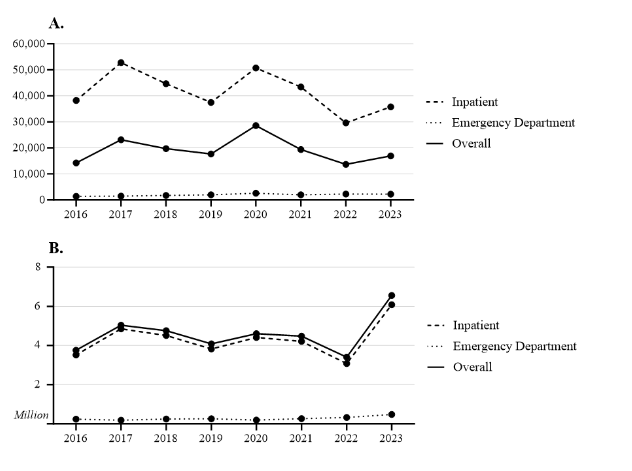 A) Mean total billed charges ($) and B) cumulative total billed charges ($, millions) for patients with lead poisoning by year and encounter type (n=1,982).
A) Mean total billed charges ($) and B) cumulative total billed charges ($, millions) for patients with lead poisoning by year and encounter type (n=1,982). Figure 2
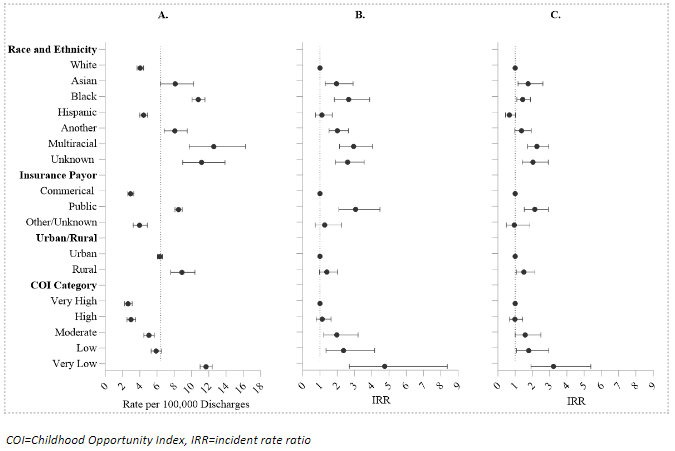 A) Crude rate of encounters for lead poisoning by patient sociodemographic factors, B) unadjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, and C) adjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, inpatient and emergency department, 2016-2023 (n=1,982).
A) Crude rate of encounters for lead poisoning by patient sociodemographic factors, B) unadjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, and C) adjusted incidence rate ratios by patient sociodemographic factors accounting for within-hospital state variation, inpatient and emergency department, 2016-2023 (n=1,982).
