Asthma 1
Session: Asthma 1
467 - Parent Perspectives of virtual asthma specialist care for pediatric asthma patients for aftercare from an emergency department visit.
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 467.5619
Kathryn Pade, Rady Children's Hospital San Diego, San Diego, CA, United States; Bahareh Ravandi, Children's Hospital Los Angeles, Los Angeles, CA, United States; Roxana Delgado-Martinez, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Estefania Ramires-Sanchez, University of California, Los Angeles David Geffen School of Medicine, Sacramento, CA, United States; Alexandra M.. Klomhaus, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Jeanine E. Hall, Children's Hospital Los Angeles, Los Angeles, CA, United States; Ray Cheung, Breathium, Pasadena, CA, United States; Todd Chang, Children's Hospital Los Angeles, Los Angeles, CA, United States; Sande Okelo, UCLA Mattel Childrens Hospital, CULVER CITY, CA, United States

Kathryn Pade, M.D. (she/her/hers)
Associate Professor of Pediatrics
Rady Children's Hospital San Diego
Rady Children's Hospital
San Diego, California, United States
Presenting Author(s)
Background: Our prior work has shown that short term use of short-message-services (SMS) to deliver post-ED AT-ASC is acceptable and appropriate among low socioeconomic and minoritized pediatric patients and caregivers. However, the utility of long-term AT-ASC in these populations is unknown.
Objective: To examine parent ratings of AT-ASC over the course of 1-year post-ED visit for child’s asthma, and to explore the association between AT-ASC ratings and baseline sociodemographic or clinical factors.
Design/Methods: This is a secondary analysis of data collected June 2022 – August 2024 in a 1-year randomized clinical trial of post-discharge AT-ASC for children who presented for ED asthma care. AT-ASC involved: 1) asthma severity assessments every 3 weeks; 2) automated treatment plans based on adherence to controller medicines and asthma severity; and 3) asthma specialist prescribing of controller medications (intervention only). Feedback on AT-ASC was obtained through quarterly telephone calls with study parents.
Results: There were 145 participants (control = 68; intervention = 77) initially enrolled with a mean age of 6.5 years. There were no significant sociodemographic or clinical differences between treatment groups (Table 1). Among all participants, there was significant asthma morbidity reported in the year prior to study enrollment, including 2+ urgent care visits (30%), 2+ ED visits (46%), 1+ hospitalizations (30%) and 2+ oral steroids (35%) (Table 2). Despite this, only 28% of all patients reported controller medication use and 19% reported prior asthma specialist care. At 9 months post-enrollment, parents (n=78) reported that the AT-ASC provided: was easy (96%), very useful (92%), met their needs (85%), and others would like it (90%), with no significant difference between control and intervention groups (Table 3). Parents with lower education were more likely to find that the AT-ASC saved time and met their needs (p < 0.05). There were no significant differences in parental perspectives of the AT-ASC for race, language, gender, income, asthma severity, number of prior ED visits, hospitalizations or steroid use (p>0.05). The intervention group (n=46) were overall very satisfied with the medical care received (94%).
Conclusion(s): Asynchronous telemedicine asthma specialist care (AT-ASC) is a viable long-term post-ED care modality for parents of children with asthma. The long-term impact of this care model on clinical outcomes needs to be evaluated prior to widespread implementation.
Table 1: Baseline Sociodemographics and Clinical Patient Characteristics at Enrollment (n=145)
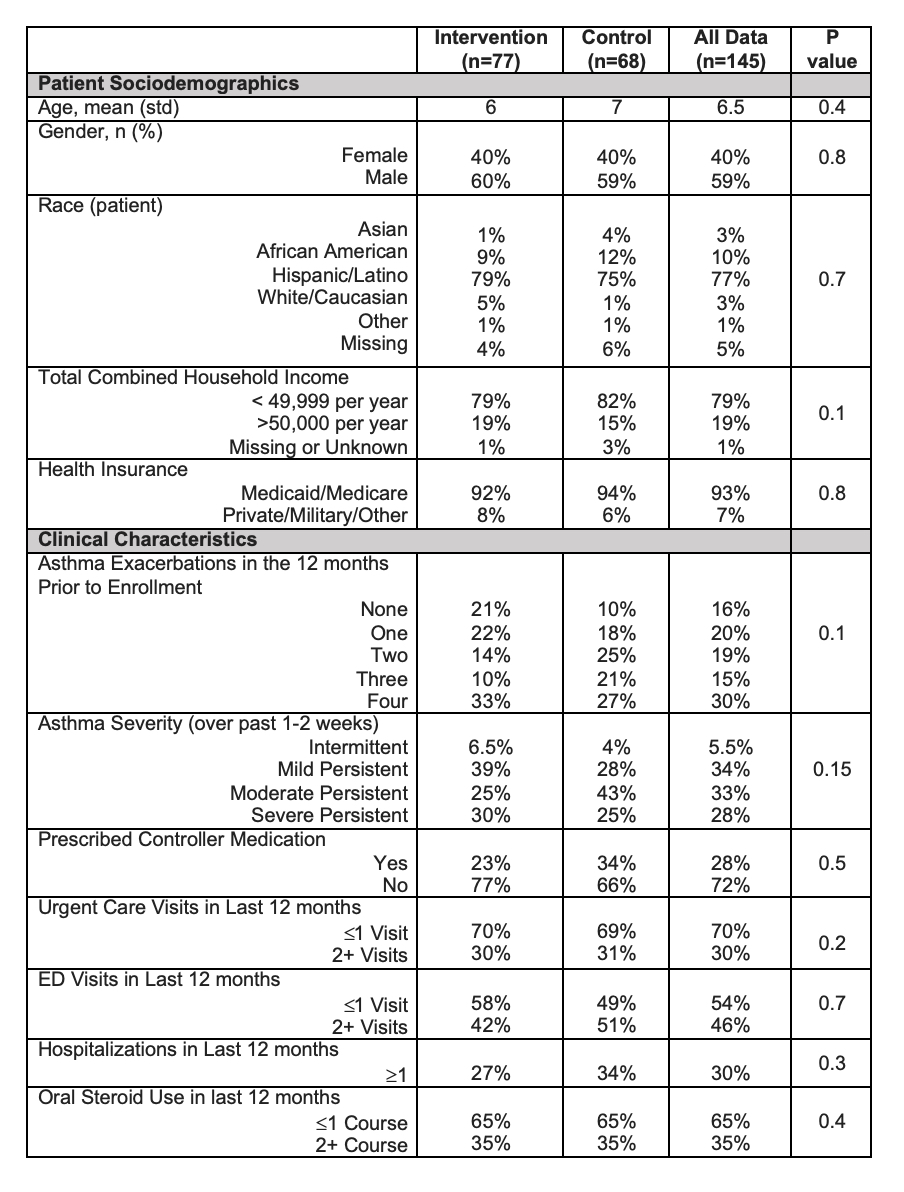
Table 2: Comparison of Virtual Asthma Care Parent Perspectives by Treatment Assignment
.jpg)
Table 1: Baseline Sociodemographics and Clinical Patient Characteristics at Enrollment (n=145)
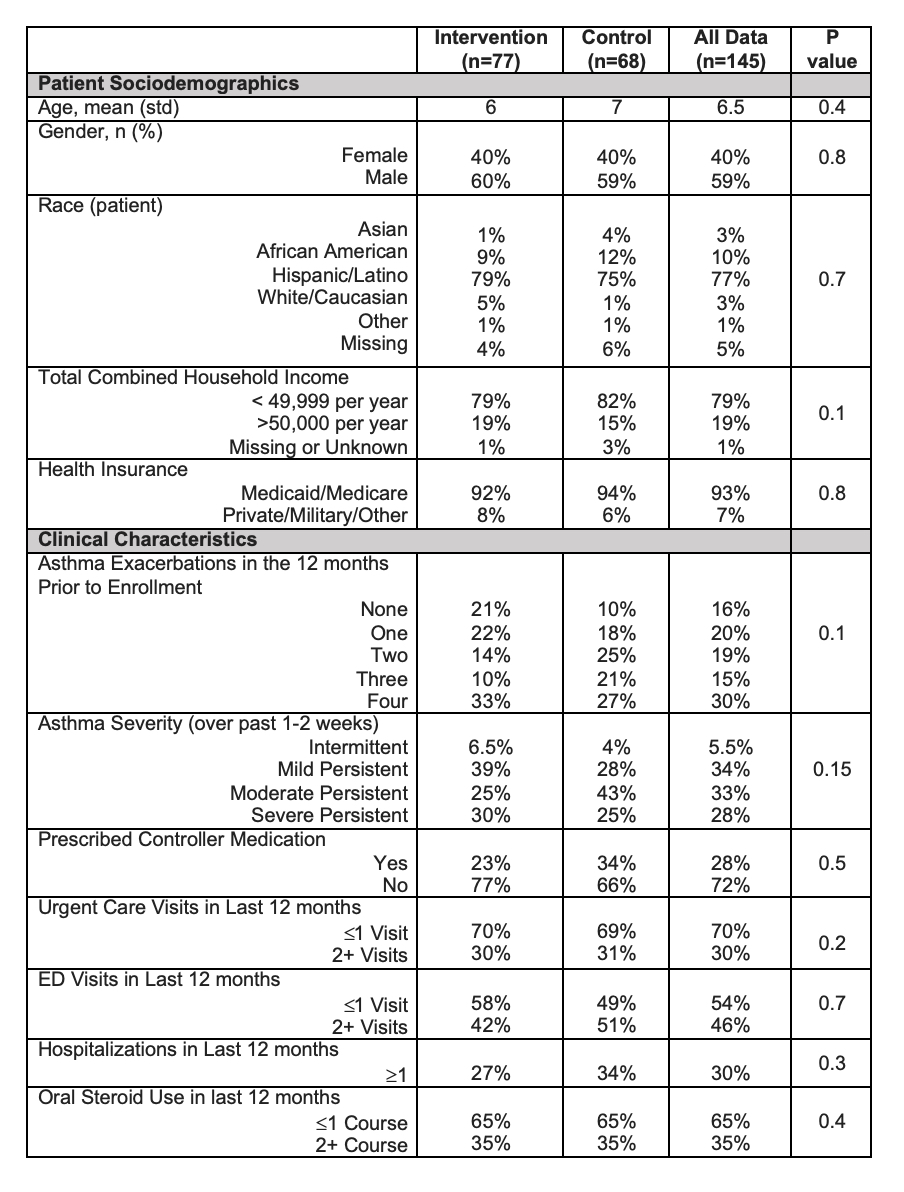
Table 2: Comparison of Virtual Asthma Care Parent Perspectives by Treatment Assignment
.jpg)

