Sedation Medicine
Session: Sedation Medicine
585 - Feasibility of Pediatric Circumcision Outside of the Operating Room using Natural Airway Sedation
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 585.4732
Juan Boriosi, University of Wisconsin-Madison, Madison, WI, United States; Michael R. Lasarev, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Walid Farhat, Division of Pediatric Urology, Madison, WI, United States; Megan Peters, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States

Juan Boriosi, MD (he/him/his)
Associate Professor of Pediatrics
University of Wisconsin-Madison
Madison, Wisconsin, United States
Presenting Author(s)
Background: Pediatric circumcision (PC) is a minor urological procedure which is often performed in an operating room (OR) setting with an artificial airway under general anesthesia. Surgeons have encountered delays in scheduling this procedure owing to increasing demand on OR resources. Other minor urological procedures have been successfully and safely performed under natural airway sedation by non-anesthesiologists in a Pediatric Sedation Unit (PSU) environment, resulting in cost savings and high rates of family satisfaction.
Objective: Our objective of this study was to transition PC from the OR to the PSU in a manner that maintained safety, efficacy, cost-effectiveness, and patient-centered care.
Design/Methods: Stakeholders in a free-leaning children’s hospital convened to plan for this new procedure in an alternative space. Following a successful transition, patient demographics, rates of sedation failures, rates of serious sedation-related safety events, financial information, and procedure characteristics were collected to compare outcomes between PC occurring in the PSU and the OR. Families of patients in the PSU were contacted following their appointment to survey their level of satisfaction with aspects of their child’s care.
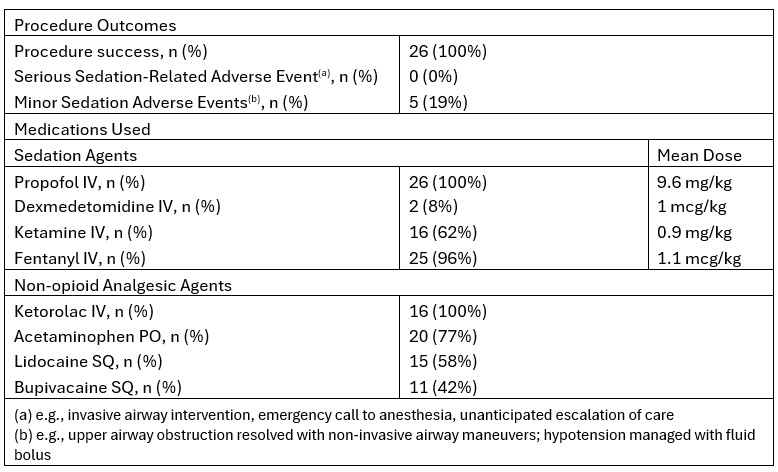
Results: Between 10/2021 and 1/2024 there were 26 PC performed by 3 urologists and 1 sedationist in the PSU. During that same period there were 125 PC in the OR. Patients in the PSU were of similar ages compared with those in the OR (median 1.90 years vs 1.68 years, P=0.95). Patients in the PSC were more likely to have an American Society of Anesthesiologist (ASA) rating of I (85% vs 62%, P=0.025). Procedures in the PSU were shorter than those occurring in the OR (32.5 min vs 77.0 min, p< 0.001), though length of stay between the two groups was statistically the same. While costs were lower for procedures in the PSU compared with the OR, so were charges and reimbursement, though the average percentage of charges collected for patients in the PSU was greater. All procedures performed in the PSU were successful using propofol with an intravenous analgesic agent and subcutaneous local anesthetic. All sedation-related adverse events were minor and reversible by the sedation team. Half of families responded to a post-PSU survey, and all families were satisfied with the care their child received.
Conclusion(s): PC can be performed in a PSU under the direction of non-anesthesiologists skilled in natural airway sedation. This procedure can be performed safely, efficiently, and at reduced cost outside of an OR setting.
Table 1. Comparison of demographics, efficiency, and financial outcomes between patients in the Pediatric Sedation Clinic and the Operating Room between 10/2021-1/2024
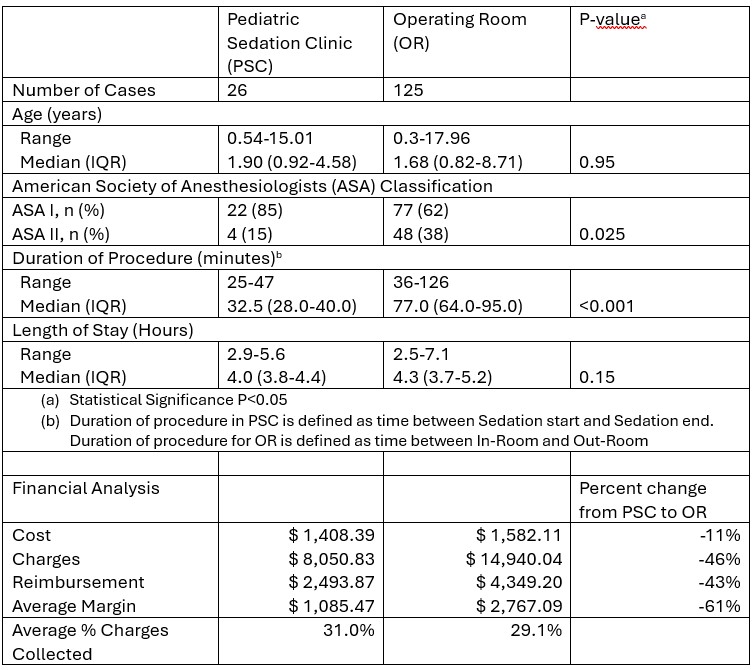
Table 2. Procedural characteristics for Circumcisions occurring in the Pediatric Sedation Clinic