Nephrology 4
Session: Nephrology 4
605 - 10 Year Kidney Outcomes & Healthcare Utilization in a Cohort of Pediatric Patients with Severe AKI by Subphenotype
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 605.3991
Zachary A. Rumlow, University of Michigan Medical School, Ann Arbor, MI, United States; Alithea Zorn, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Jason M. Misurac, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Amy Strong, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States

Amy Strong, MD MSCE (she/her/hers)
Instructor of Pediatrics - Nephrology
University of Iowa Stead Family Children's Hospital
Iowa City, Iowa, United States
Presenting Author(s)
Background: Recognizing AKI subphenotypes is crucial for understanding the diverse mechanisms and outcomes associated with AKI. This classification can lead to more personalized and effective management strategies for children with AKI, potentially improving their long-term health outcomes. However, literature on these subphenotype differences is limited.
Objective: This study aimed to describe the differences in 10-year kidney outcomes and healthcare utilization by clinical subphenotype of AKI in a cohort of patients hospitalized in a PICU.
Design/Methods: Children and young adults admitted to a single tertiary care PICU in 2013 were eligible, excluding those with end-stage kidney disease or significant CKD. 10-year follow-up data was collected through December 2023. AKI was defined from all creatinine data obtained during the index admission using the KDIGO criteria. Clinical subphenotypes were assigned upon review of medical records. Subphenotypes included sepsis-associated, nephrotoxic medication, hemato-oncologic, cardiac, primary renal, and other. AKI events could be classified into multiple subphenotypes if appropriate. Outcomes of interest included long-term kidney outcomes (renal recovery, subsequent AKI events, CKD, proteinuria, and hypertension) and healthcare utilization (admission duration and subsequent inpatient days) by subphenotype.
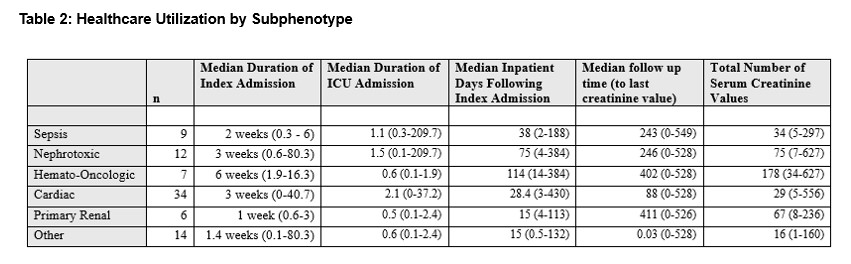
Results: Of the 595 eligible patients, 63 (11%) met criteria for severe (at least stage II) AKI. The median age of those with AKI was 4.8 years. 49% had stage II AKI and 51% had stage III AKI. 4% of those with severe AKI died during the admission. The most common AKI subphenotype was cardiac in 34/82 (41%) of those classified. Eleven of those with severe AKI had CKD (17%) at maximum follow-up. Long-term kidney outcomes by subphenotype are detailed in table 1. Healthcare utilization outcomes by subphenotype are detailed in table 2.
Conclusion(s): This study highlights the significant variability in long-term kidney outcomes and healthcare utilization among different AKI subphenotypes in pediatric patients. The findings underscore the importance of recognizing and classifying AKI subphenotypes to tailor management strategies more effectively. The observed differences in outcomes, particularly the high prevalence of CKD in certain subphenotypes, emphasize the need for ongoing monitoring and targeted interventions. Further research is essential to deepen our understanding of these subphenotypes and to develop optimized, personalized treatment protocols that can improve long-term health outcomes for children affected by AKI.
Long Term Kidney Outcomes by Subphenotype
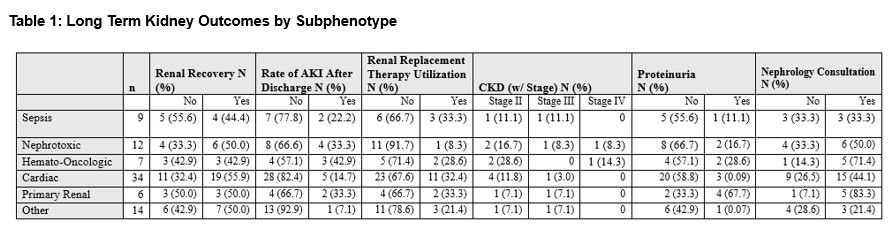
Healthcare Utilization by Subphenotype