Newborn Care 2
Session: Newborn Care 2
265 - Maternal Risk Factors for NICU Admission Among Term Appropriate for Gestational Age (AGA) Infants.
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 265.5873
Sarah M. Sanchez, Maria Fareri Children's Hospital at Westchester Medical Center, Fort Lee, NJ, United States; Heather L. Brumberg MD, MPH, New York Medical College, Maria Fareri Children’s Hospital @ Westchester Medical Center, White Plains, NY, United States; Elissa Dunlap, New York Medical College, New York, NY, United States; Clare Giblin BSN-NIC, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; Shetal Shah, Maria Fareri Children's Hospital at Westchester Medical Center, Syosset, NY, United States
- SS
Sarah M. Sanchez, MD, FAAP (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Maria Fareri Children's Hospital at Westchester Medical Center
Fort Lee, New Jersey, United States
Presenting Author(s)
Background: Although full term infants comprise ~1/3-1/2 of all US NICU admissions and thus consume a disproportionate share of resources, they are an understudied population. The few available studies include small for gestational age (SGA) and large for gestational age (LGA) infants, both independent risk factors for NICU admission. However, little is known regarding characteristics of term AGA NICU admissions (AGA TERM NICU), including maternal clinical and social contributors such as adverse life events known to impact newborn care.
Objective: To determine maternal risk factors for AGA TERM NICU.
Design/Methods: This is a cross-sectional study (2016-2023) of maternal (≥18 yrs) survey responses merged with birth certificate data of singleton live births. AGA TERM NICU was defined as an infant admitted to the NICU at gestational age >37 weeks as per birth certificate data. Those with significant congenital anomalies & SGA & LGA infants (based on the 2013 Fenton growth charts) were excluded. Maternal characteristics included demographics, adverse life events [ALE ≥3 of 14 stressors such as homelessness or incarceration], lifestyle behaviors & pregnancy history. Bivariate and multivariate analysis was performed. Logistic regression included nativity, self-reported race/ethnicity, pregnancy and preconception conditions, mental health, substance use, delivery mode & other social factors. Obesity was not included due to collinearity with gestational diabetes.
Results: 1073 mothers were analyzed of which 90 had AGA TERM NICU. Compared with mothers of AGA term well-baby nursery admission (AGA TERM WBN), mothers with AGA TERM NICU admission differed by self-reported race, exhibited lower rates of prenatal care, had higher rates of both foreign birth & gestational diabetes (Table 1). Cesarean delivery, gestational diabetes & self-identified Non-Hispanic Black race exhibited higher odds of AGA TERM NICU compared with AGA TERM WBN (Table 2). The model accurately predicted 69% of AGA TERM NICU (receiver operator curve with concordance index =0.69).
Conclusion(s): This is the first study to examine maternal factors associated with AGA TERM NICU. Cesarean delivery, gestational diabetes, and self-reported Non-Hispanic Black race was associated with AGA TERM NICU. We speculate these results may identify opportunities for intervention and additional supports to reduce rates of AGA TERM NICU, especially regarding stressors such as racism, maternal clinical conditions and delivery mode.
Table 1: Demographics of Mothers with AGA Term NICU Admission.
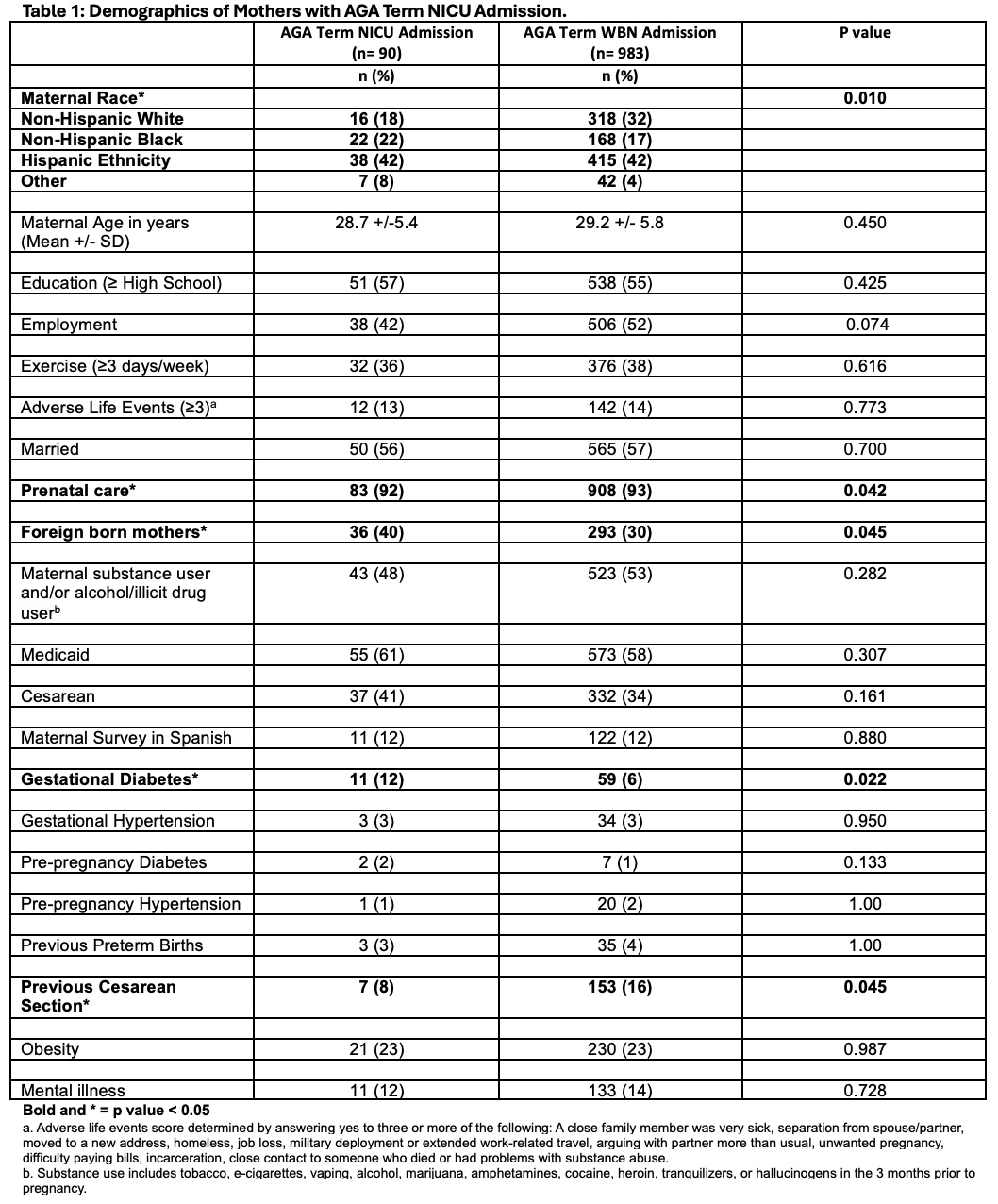
Table 2: Odds Ratio: Maternal Risk Factors and AGA Term NICU Admission.
.jpg)

