Asthma 2
Session: Asthma 2
481 - Long-term viability of asynchronous telemedicine to improve access to asthma specialist care following an emergency department (ED) asthma visit
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 481.5764
Bahareh Ravandi, Children's Hospital Los Angeles, Los Angeles, CA, United States; Jeanine E. Hall, Children's Hospital Los Angeles, Los Angeles, CA, United States; Kathryn Pade, Rady Children's Hospital San Diego, San Diego, CA, United States; Estefania Ramires-Sanchez, University of California, Los Angeles David Geffen School of Medicine, Sacramento, CA, United States; Alexandra M.. Klomhaus, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Todd Chang, Children's Hospital Los Angeles, Los Angeles, CA, United States; Roxana Delgado-Martinez, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Ray Cheung, Breathium, Pasadena, CA, United States; Sande Okelo, UCLA Mattel Childrens Hospital, CULVER CITY, CA, United States

Bahareh Ravandi, MD
Clinical Assistant Professor of Pediatrics
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Few high-risk pediatric patients with uncontrolled asthma ever receive guideline-recommended care to improve outcomes due to low rates of post-emergency department (ED) follow-up care with primary care providers as well as other access barriers. We developed a SMS text message-based asynchronous telemedicine asthma specialist care program (AT-ASC) for post-ED care. Previously, we showed AT-ASC as a viable short-term strategy, with an average of 3 completed AT-ASC visits during the first 3 months post-ED visit. The long-term viability of AT-ASC is unknown.
Objective: We sought to evaluate the viability of AT-ASC on meeting guideline recommendations for post ED asthma specialist care visits for 1 year following the index ED visit for asthma.
Design/Methods: This is a secondary analysis of data collected during a randomized clinical trial of AT-ASC among children presenting for asthma care in the ED (June 2022 - August 2024). We offered prospective participants: 1) post-ED asthma surveys via SMS every 3 weeks for 1 year, with automated feedback on severity level and preliminary acute treatment suggestions. Intervention participants also received: 2) asthma severity assessment during the ED visit; 3) weekly alerts by SMS when pollution levels indicated a high risk of asthma attacks; 4) initiation of controller medications by a pediatric pulmonologist within 24 hours of the ED visit with adjustments based on AT-ASC visit findings. We examined the frequency of completed AT-ASC visits over a 1-year period, and if there was an association with baseline sociodemographic and clinical factors.
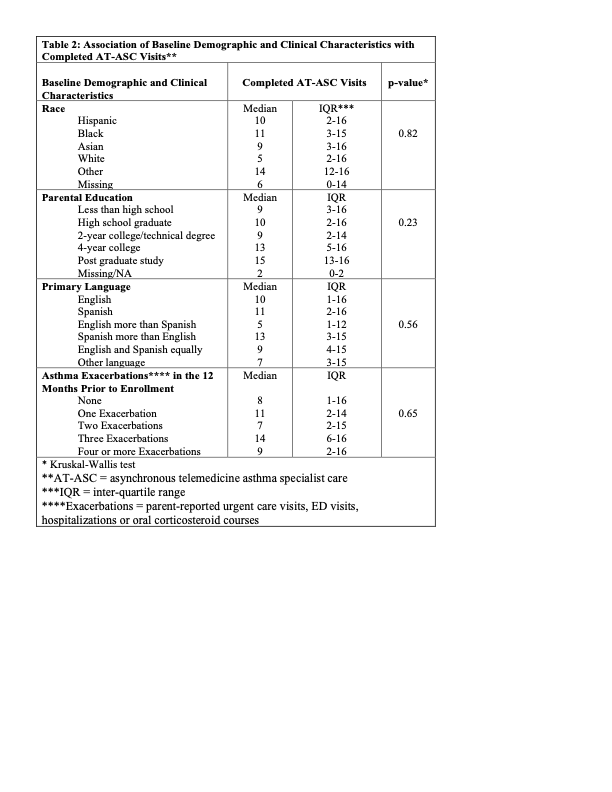
Results: 145 participants were enrolled (control = 68; intervention = 77), primarily from under-served populations (table 1). Despite significant asthma morbidity reported in the year prior to study enrollment (figure 1), nearly three-fourths reported no controller medication use. More than 80% desired to see an asthma specialist, while only 20% had ever seen one—only half were seen within the last year. During the 1-year post-ED follow-up period, 86% of participants completed at least one AT-ASC visit (median [IQR] = 11 [4-16]). While 66% completed 4 or more visits (median [IQR] = 14 [10-16]). The number of completed AT-ASC visits did not vary by baseline sociodemographic or clinical characteristics (table 2).
Conclusion(s): AT-ASC is a viable long-term strategy for asthma specialist care following an ED encounter for asthma. Additional research is needed to determine the effects on the capacity of asthma specialist care and on clinical outcomes.
Table 1: Baseline Participant Sociodemographic Characteristics
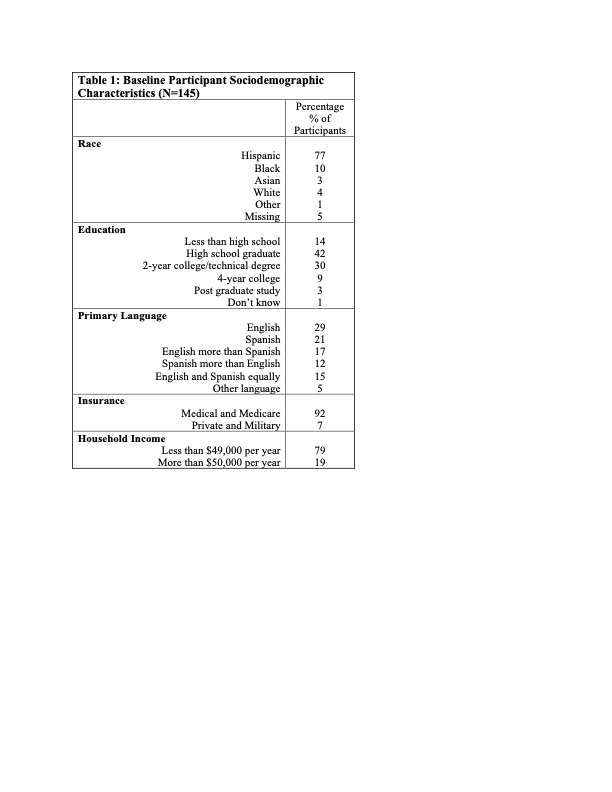
Figure 1: Asthma morbidity year prior to enrollment
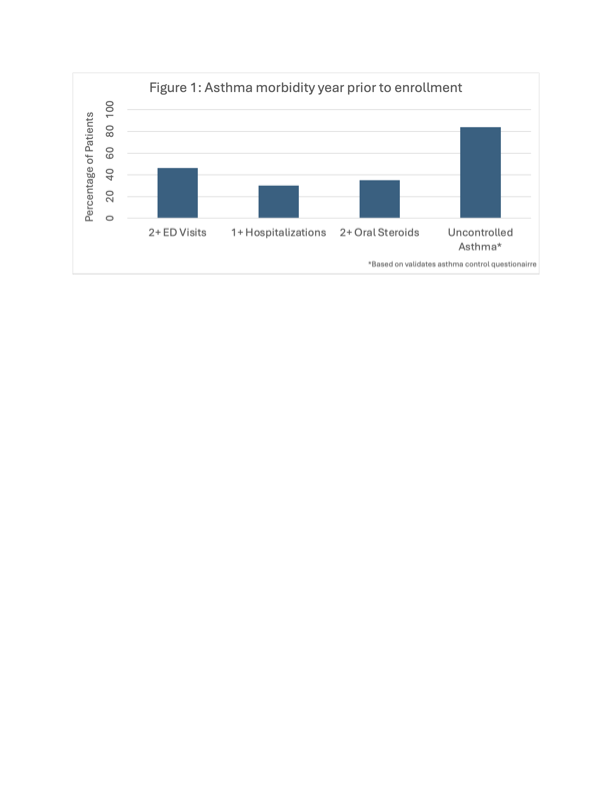
Table 2: Association of Baseline Demographic and Clinical Characteristics with Completed AT-ASC Visits