Back
Background: Caring for pediatric patients at the end-of-life (EOL) is a high acuity, low occurrence, and often distressing clinical scenario. The complex social and medical needs of dying pediatric patients and their families are best served by skilled interprofessional teams. Pediatric trainees rarely receive formal EOL skills training as part of their education, yet participate in the care of critically ill and dying children.
Objective: The pediatric end-of-life care skills (PECS) interprofessional workshop was developed to address a well-described education gap and provide a structured opportunity to build and practice the skills required for effective pediatric EOL care.
Design/Methods: The PECS workshop was developed by an interprofessional workgroup, including bereaved parent faculty. Participants of the PECS workshop included pediatrics and medicine pediatrics residents, pediatric nurse practitioner students, masters of social work students, early career multidisciplinary members who were recruited via email. The workshop was developed using the principles of deliberate practice. Participants completed a single post-workshop survey that assessed key knowledge elements and self-reported competencies in providing EOL care. Responses on knowledge based questions before vs after the workshop were rescored to indicate decreased, stable, or increased knowledge. Responses were summarized with count (%) and visualized with stacked bar plots. Participants had the option to complete a free response portion on the survey. Preliminary inductive qualitative content analysis was conducted on free response questions. Only first-time participants were included in the analysis.
Results: 78 interprofessional trainees participated across 8 pilot PECS workshops, held over 2 years. All participants completed surveys. Survey self-assessment remained stable or improved before vs after the workshop in nearly all domains (Figure 1) across disciplines. Key emerging themes of knowledge that participants gained and intend to use in ongoing clinical practice include: importance and mechanics of interprofessional teamwork, the power of silence, and new communication skills including specific language to use in difficult conversations and emotional responses.
Conclusion(s): Interprofessional PECS workshops are an effective educational tool to improve individual confidence and self-reported competence in EOL care skills across disciplines and to build interprofessional skills in caring for critically ill and dying children. Further work will explore workshop sustainability and application and durability of learned skills in clinical practice.
Figure 1
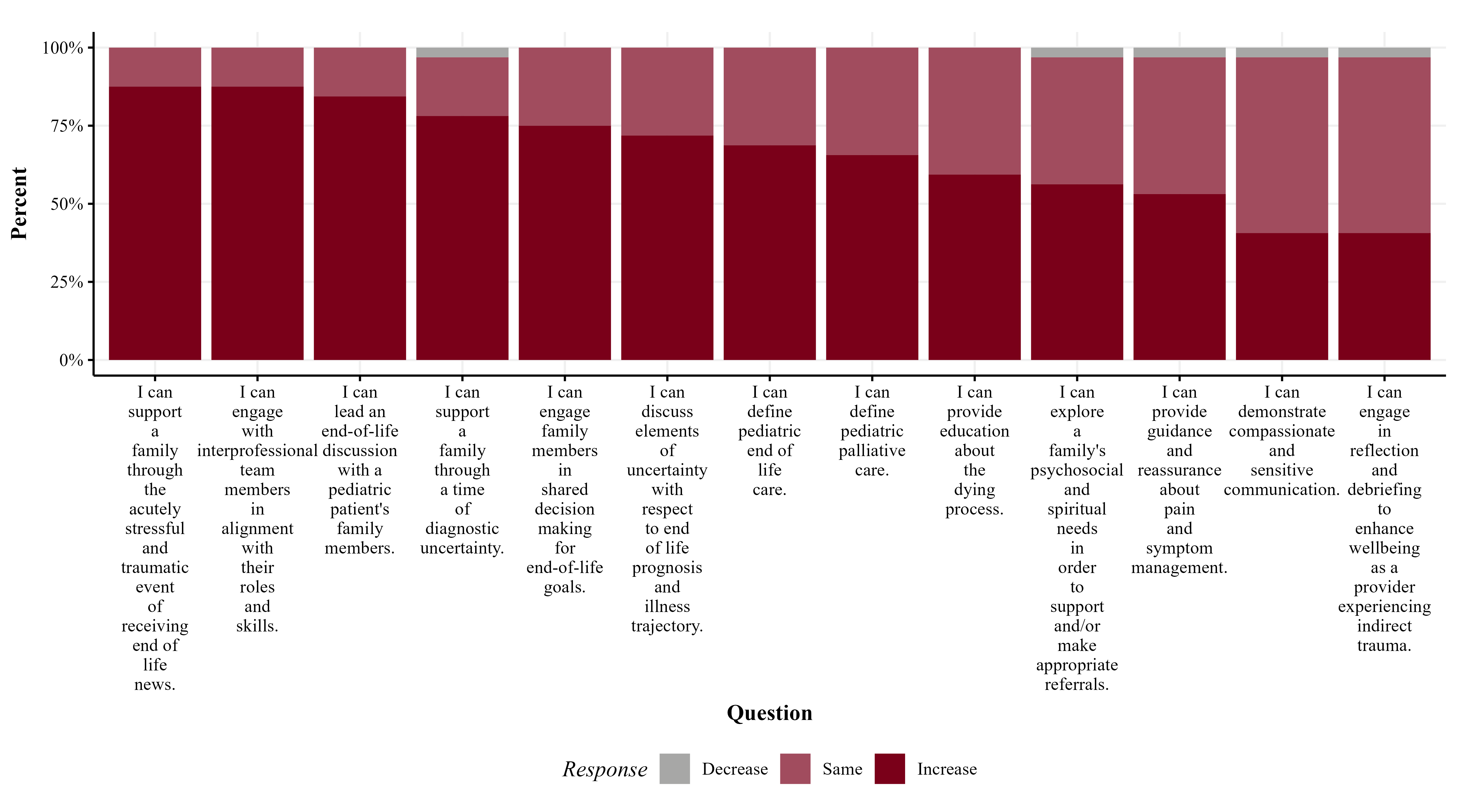 End of Life Care Skill Domains: change in self assessed skill level in pediatric EOL care domains before vs. after workshop participation
End of Life Care Skill Domains: change in self assessed skill level in pediatric EOL care domains before vs. after workshop participation
Palliative Care
Session: Palliative Care
436 - Pediatric End-of-Life Skills: An Interprofessional Workshop to Bridge Education Gap
Sunday, April 27, 2025
8:30am – 10:45am HST
Alyssa Levine, University of Minnesota Masonic Children's Hospital, Minneapolis, CA, United States; Kirsten Kreh, University of Minnesota Medical School, Saint Paul, MN, United States; Rebecca Freese, University of Minnesota, Minneapolis, MN, United States; Susan K. O Conner Von, University of Minnesota, Saint Paul, MN, United States; Miriam C. Shapiro, University of Minnesota Medical School, Minneapolis, MN, United States; Stacy S.. Remke, University of Minnesota, St Paul, MN, United States; Johannah M. Scheurer, University of Minnesota, Minneapolis, MN, United States; Anne Woll, University of Minnesota, Minneapolis, MN, United States; Kelly McManimon, University of Minnesota Masonic Children's Hospital, Stillwater, MN, United States; Dannell Shu, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States

Alyssa Levine, MD (she/her/hers)
Fellow
University of Minnesota Masonic Children's Hospital
Minneapolis, California, United States
Presenting Author(s)
Background: Caring for pediatric patients at the end-of-life (EOL) is a high acuity, low occurrence, and often distressing clinical scenario. The complex social and medical needs of dying pediatric patients and their families are best served by skilled interprofessional teams. Pediatric trainees rarely receive formal EOL skills training as part of their education, yet participate in the care of critically ill and dying children.
Objective: The pediatric end-of-life care skills (PECS) interprofessional workshop was developed to address a well-described education gap and provide a structured opportunity to build and practice the skills required for effective pediatric EOL care.
Design/Methods: The PECS workshop was developed by an interprofessional workgroup, including bereaved parent faculty. Participants of the PECS workshop included pediatrics and medicine pediatrics residents, pediatric nurse practitioner students, masters of social work students, early career multidisciplinary members who were recruited via email. The workshop was developed using the principles of deliberate practice. Participants completed a single post-workshop survey that assessed key knowledge elements and self-reported competencies in providing EOL care. Responses on knowledge based questions before vs after the workshop were rescored to indicate decreased, stable, or increased knowledge. Responses were summarized with count (%) and visualized with stacked bar plots. Participants had the option to complete a free response portion on the survey. Preliminary inductive qualitative content analysis was conducted on free response questions. Only first-time participants were included in the analysis.
Results: 78 interprofessional trainees participated across 8 pilot PECS workshops, held over 2 years. All participants completed surveys. Survey self-assessment remained stable or improved before vs after the workshop in nearly all domains (Figure 1) across disciplines. Key emerging themes of knowledge that participants gained and intend to use in ongoing clinical practice include: importance and mechanics of interprofessional teamwork, the power of silence, and new communication skills including specific language to use in difficult conversations and emotional responses.
Conclusion(s): Interprofessional PECS workshops are an effective educational tool to improve individual confidence and self-reported competence in EOL care skills across disciplines and to build interprofessional skills in caring for critically ill and dying children. Further work will explore workshop sustainability and application and durability of learned skills in clinical practice.
Figure 1
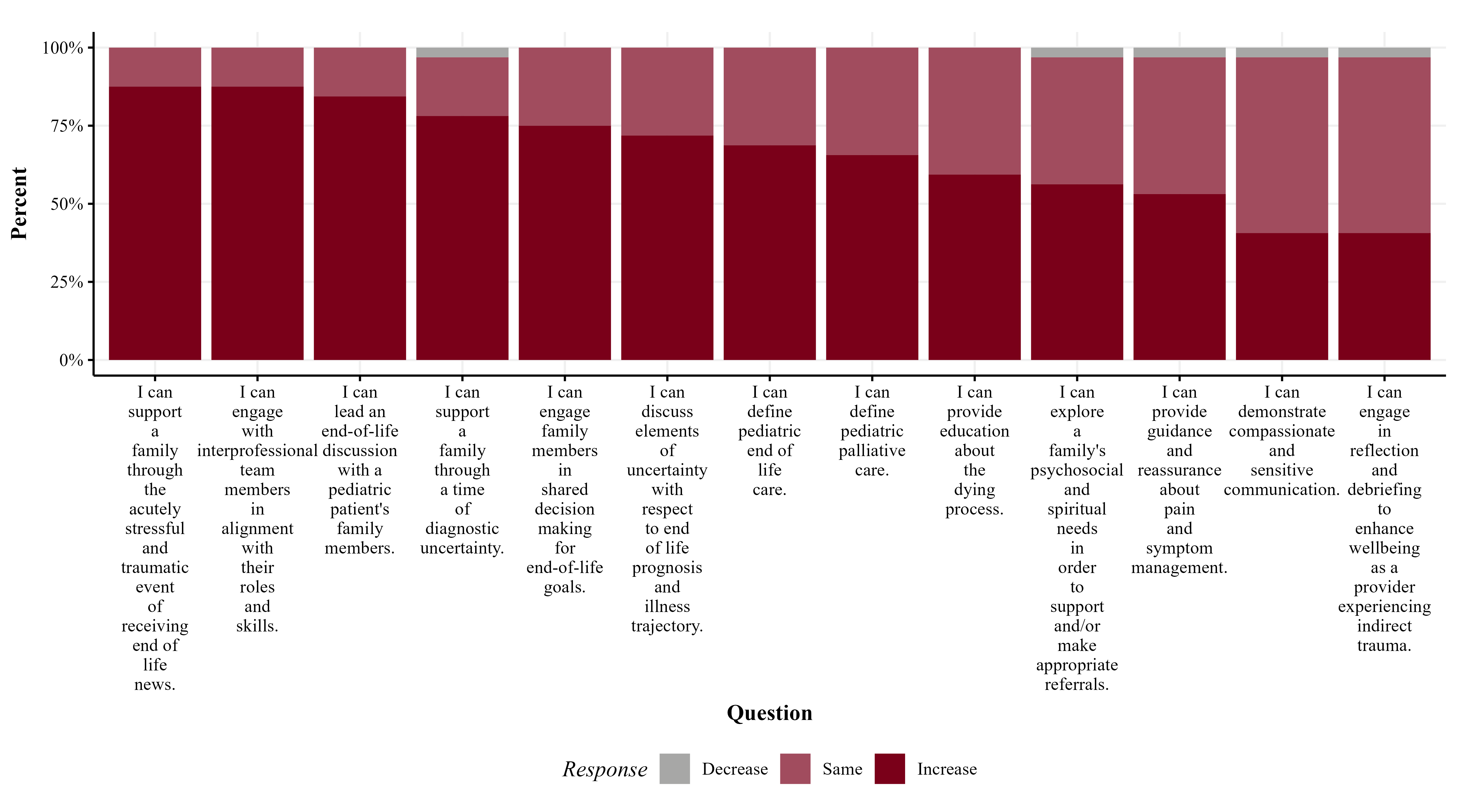 End of Life Care Skill Domains: change in self assessed skill level in pediatric EOL care domains before vs. after workshop participation
End of Life Care Skill Domains: change in self assessed skill level in pediatric EOL care domains before vs. after workshop participation
