Palliative Care
Session: Palliative Care
439 - Barriers and facilitators to interdisciplinary pediatric palliative care collaboration
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 439.3806
Maureen M. Kemna, University Medical Center Utrecht, Utrecht, Utrecht, Netherlands; Judith Aris-Meijer, Uiversity Medical Center Groningen, Groningen, Groningen, Netherlands; Eduard Verhagen, University Medical Center Groningen, Groningen, Groningen, Netherlands; Saskia Teunissen, University Medical Center Utrecht, Utrecht, Utrecht, Netherlands; Marijanne Engel, University Medical Center Utrecht, Utrecht, Utrecht, Utrecht, Netherlands; Marijke C. Kars, UMCUtrecht, Utrecht, Utrecht, Netherlands

Maureen M. Kemna, MD (she/her/hers)
PhD student
University Medical Center Utrecht
Utrecht, Utrecht, Netherlands
Presenting Author(s)
Background: Children receiving pediatric palliative care (PPC) increasingly reside and die at home. This shift necessitates close collaboration among three key groups: 1) parents, who bring unique expertise into their child’s needs and family dynamics; 2) academic healthcare professionals (HCPs), specialized in rare and complex conditions; and 3) home care HCPs, who support daily life with a condition. In PPC, this collaboration occurs within so-called Situational Care Networks (SCNs), i.e. the partnership between parents and HCPs involved in caring for the child and family. Interdisciplinary collaboration (IDC) within SCNs is crucial, but encounters challenges.
Objective: This study aims to identify barriers and facilitators to IDC in SCNs, as perceived by both parents and HCPs.
Design/Methods: A multiple case study was conducted in SCNs, using semi-structured interviews with (bereaved) parents of children who primarily live(d) at home, and their HCPs. Bereaved parents whose child had died more than six months before the interview were excluded from participation. Data was analyzed thematically.
Results: Fourteen parents and thirty-nine HCPs across nine SCNs participated. Eleven barriers to IDC were identified and could be categorized into three overarching domains (Table 1): a lack of organization and management of IDC, obstructive perceptions among collaborative partners, and personal needs and interests of collaborative partners. Parents frequently felt compelled to take on tasks and responsibilities that HCPs had not addressed.
Similarly, ten facilitators were identified, also categorized into three overarching domains (Table 2): organization and management of IDC, active enhancement and support of collective expertise, and personal characteristics of collaborative partners. IDC improved during the child’s terminal phase as urgency increased, consensus on comfort care was reached, and the family’s needs were prioritized as main goals.
Conclusion(s): IDC within SCNs encounters several challenges, primarily related to the limited awareness of the SCN’s existence, the failure to recognize the added value of each members’ expertise, and the underappreciation of IDC’s benefits. These issues frequently place excessive organizational burdens on parents, leading to a need for control. Improvements can be achieved by initiating IDC earlier, raising awareness of each member’s unique contribution to the SCN, and actively communicating with parents what support they need to achieve their desired level of control, as well as patient-centered care.
Table 1 Selected quotes illustrating perceived barriers of parents and HCPs for interdisciplinary collaboration in PPC’s situational care networks
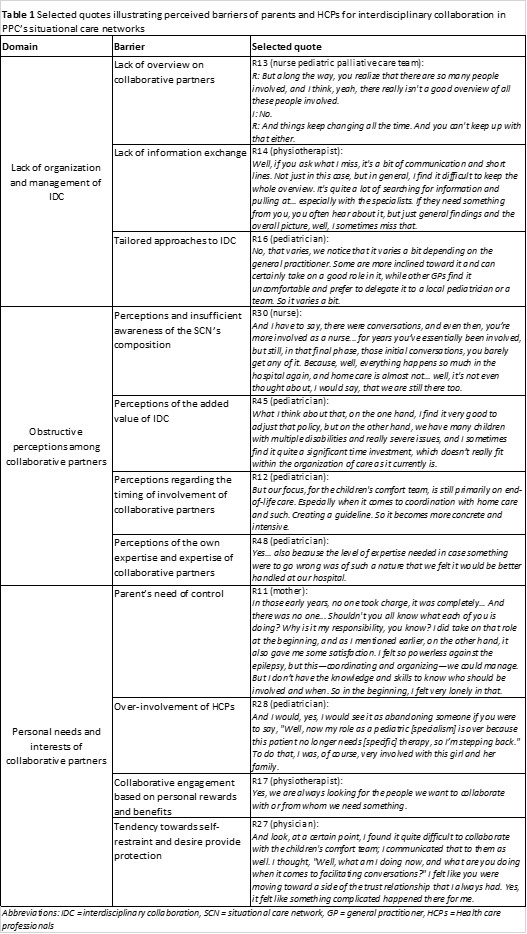 Abbreviations: IDC = interdisciplinary collaboration, SCN = situational care network, GP = general practitioner, HCPs = Health care professionals
Abbreviations: IDC = interdisciplinary collaboration, SCN = situational care network, GP = general practitioner, HCPs = Health care professionalsTable 2 Selected quotes illustrating perceived facilitators of parents and HCPs for interdisciplinary collaboration in PPC’s situational care networks
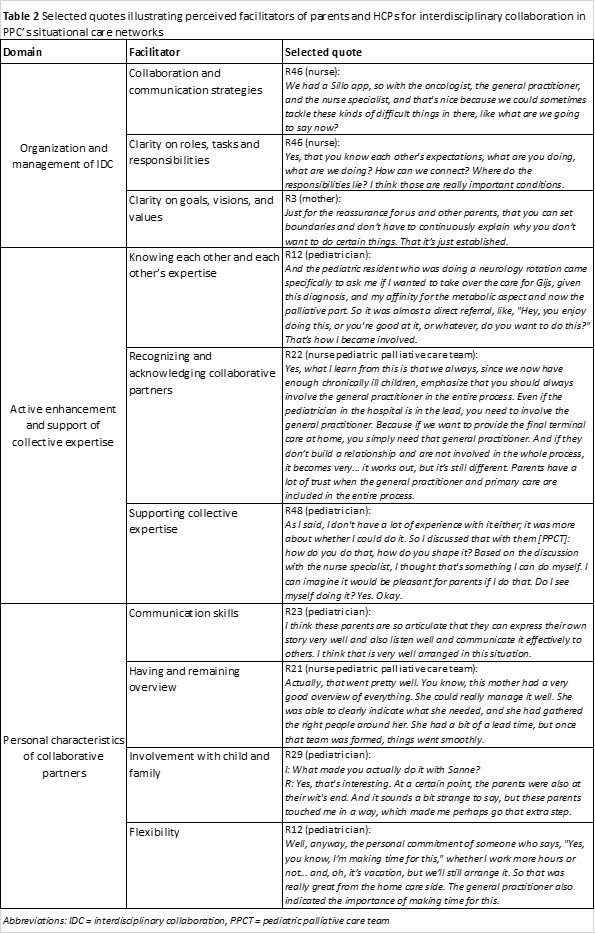 Abbreviations: IDC = interdisciplinary collaboration, PPCT = pediatric palliative care team
Abbreviations: IDC = interdisciplinary collaboration, PPCT = pediatric palliative care team
