Nephrology 6
Session: Nephrology 6
636 - Nephrocalcinosis in Pediatric Kidney Transplantation: Insights into Mineral Dysregulation
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 636.5740
Yaritzy M. Astudillo, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Debora Matossian, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Priya S. Verghese, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Stella Kilduff, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
- YA
Yaritzy M. Astudillo, MD (she/her/hers)
Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Nephrocalcinosis in the post-kidney transplant setting is common occurring in up to 30% within 3 months. While adult studies have shown an association with poor overall graft function, the risks and causes of calcium deposition remain unclear and poorly described in pediatrics.
Objective: To analyze calcium-phosphorus metabolism and identify predisposing factors from the medical history and clinical course of pediatric kidney transplant recipients (KTRs) with biopsy-confirmed calcium depositions. We hypothesized that predisposing factors may include elevated calcium and parathyroid hormone (PTH) levels pre and post-transplant.
Design/Methods: Six pediatric KTRs at a single center with calcium deposition on posttransplant kidney biopsies were included. Continuous variables are reported as either mean ± standard deviation or median (interquartile range, IQR) and categorical variables were reported as n (%).
Results: All recipients were males with an average age at transplant of 17.3 ± 2.8 years and a median time to biopsy of 54 (40, 97) days. CAKUT was the cause of ESKD in 50%. The majority of the patients were African American, underwent dialysis pre-transplant, received deceased donor grafts, and half had hematuria on screening urinalysis (Table 1). The median dialysis vintage was 462 (175, 1587) days for non-preemptive transplants. Median glomerular filtration rate (GFR) pre-biopsy was 38 mL/min/1.73m2 (29, 53).
Median PTH levels pre-transplant and pre-biopsy were 180 (119, 469) and 149 (75, 531) respectively (Table 2). The average calcium levels pre-transplant and pre-biopsy were 9.9±0.6 and 9.7±0.7 respectively. The average phosphorus levels pre-transplant and pre-biopsy were 5.6±1.0 and 3.7±1.0 respectively.
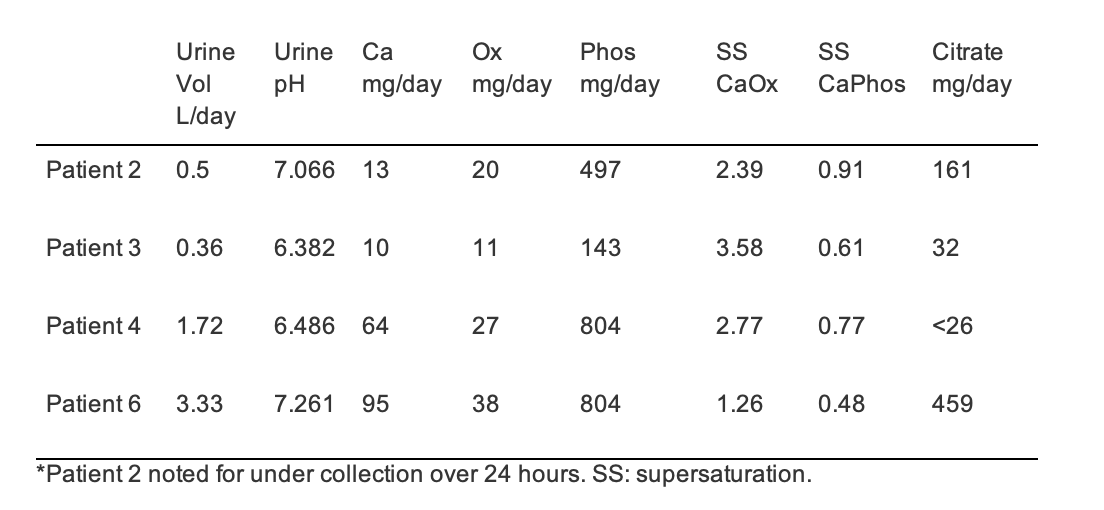
24 hour urine collections on 4 patients were significant for pH > 6.2 in all; 2 had hypocitraturia (Table 3); All patients had >4mg/day of calcium. In addition to nephrocalcinosis, some additional biopsy findings included interstitial fibrosis and tubular atrophy and capillaritis.
Conclusion(s): Most KTRs with nephrocalcinosis had normal calcium and phosphate levels, and some had normal PTH levels, suggesting a need to investigate other risk factors. Future studies will compare these patients to those without calcium deposition to assess the impact of factors like hypocitraturia and high urine pH. While limited by sample size, the significant graft dysfunction seen, suggests that calcium deposition may be a key factor. Our findings emphasize the need to manage mineral homeostasis in KTRs to mitigate the risk of nephrocalcinosis and improve long-term outcomes.
Table 1. Demographic data of kidney transplant recipients with biopsy-proven calcium deposition and donors
.png)
Table 2. Calcium Phosphorus metabolism values pre-transplant and pre-biopsy
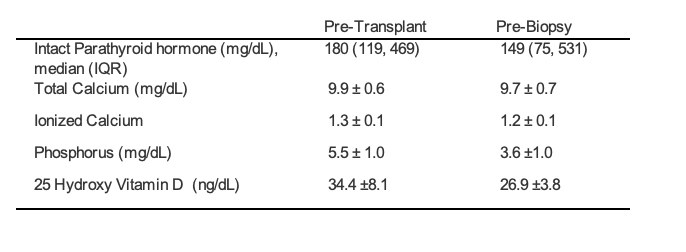
Table 3. 24 hour urine collection for kidney transplant recipients with biopsy-proven calcium deposition