Neonatal Neurology 5: Fetal
Session: Neonatal Neurology 5: Fetal
669 - A practice survey of prenatally identified supratentorial midline brain malformations
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 669.3822
Allison J. Chirigos, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Sonika Agarwal, The Children's Hospital of Philadelphia, Philadelphia, PA, United States; Betsy Ostrander, University of Utah School of Medicine, Salt Lake City, UT, United States; Marielle Young, University of Utah, Salt Lake City, UT, United States; Allison Smego, University of Utah, Salt Lake City, UT, United States; Niranjana Natarajan, University of Washington School of Medicine, Seattle, WA, United States; Marissa Vawter-Lee, Cincinnati Children's Hospital Medical Center, Cincinatti, OH, United States; Dawn Gano, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Charu Venkatesan, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Jennifer C. Keene, University of Utah, Salt Lake City, UT, United States

Allison J. Chirigos, MD (she/her/hers)
Neonatal and Fetal Neurology Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Supratentorial midline brain malformations (MBMs), a common category of prenatally-diagnosed central nervous system malformation, comprise approximately one third of fetal neurology consults. Outcomes associated with MBMs are broad and include a high risk for endocrine and ophthalmologic complications, epilepsy, cerebral palsy, intellectual disability, autism, behavioral disorders.
Objective: Our study aims to characterize the care of infants with prenatally-identified MBMs to support development of multidisciplinary care guidelines.
Design/Methods: We distributed a Redcap survey regarding management of infants with MBMs to U.S.-based pediatric neurologists who perform fetal consultations. Respondents were asked about their practice context and recommendations regarding care pre-delivery, postnatal imaging, endocrine and ophthalmologic evaluation, and developmental monitoring. Data analysis was descriptive.
Results: Twenty surveys were completed from 15 institutions across the U.S. Most (19/20, 95%) respondents perform fetal neurology consultations in a multidisciplinary setting. MBM complexity affected delivery location (11/20, 55%) and postnatal imaging recommendations (15/20, 75%). All respondents pursue endocrine evaluation for infants with certain MBMs, and 14/20 (70%) recommend unequivocal endocrine evaluation. 8/20 (40%) recommend endocrinology consultation to guide evaluation, 8/20 (40%) recommend specific screening labs in all infants, and 4/20 (20%) recommend screening labs for infants with certain MBMs. The 12/20 (60%) who recommended specific screening labs most frequently recommended TSH (12/12, 100%), free T4 (12/12, 100%), cortisol (12/12, 100%), and BMP (11/12, 92%). Most (19/20, 95%) recommend ophthalmologic evaluation for certain infants (86% refer for holoprosencephaly, 71% for complex MBMs, 57% for isolated absent septum pellucidum or isolated absence of the corpus callosum in female infants), and 12/20 (60%) recommend universal ophthalmology referral. 19/20 (95%) indicate that children referred to ophthalmology are typically seen following birth while hospitalized or within the first few weeks. Developmental monitoring through pediatric neurology clinic (16/20, 80%) and Early Intervention (13/20, 65%) was recommended for patients with any MBM.
Conclusion(s): Patients with prenatally-identified MBMs require a multidisciplinary approach, including endocrine and ophthalmologic evaluations and developmental monitoring, to optimize neurodevelopmental outcomes and facilitate early diagnosis of medical complications. Results of this survey may inform a standardized approach to care.
Postnatal imaging recommendations based on type of MBM.
.jpg) 5/20 (25%) of survey respondents make the same imaging recommendations regardless of MBM type, with 4 recommending postnatal imaging unconditionally, and 1 recommending imaging conditionally based on the timing of the prenatal magnetic resonance imaging. The other 15/20 (75%) of survey respondents state that their postnatal imaging recommendations differ based on the patient’s MBM type, and this bar graph depicts their recommendations. The green bars represent the number of those 15 providers who recommend cranial ultrasound (CUS), and the blue bars represent the number who recommend magnetic resonance imaging (MRI) for each type of MBM.
5/20 (25%) of survey respondents make the same imaging recommendations regardless of MBM type, with 4 recommending postnatal imaging unconditionally, and 1 recommending imaging conditionally based on the timing of the prenatal magnetic resonance imaging. The other 15/20 (75%) of survey respondents state that their postnatal imaging recommendations differ based on the patient’s MBM type, and this bar graph depicts their recommendations. The green bars represent the number of those 15 providers who recommend cranial ultrasound (CUS), and the blue bars represent the number who recommend magnetic resonance imaging (MRI) for each type of MBM.Endocrine evaluation recommended for patients with MBMs.
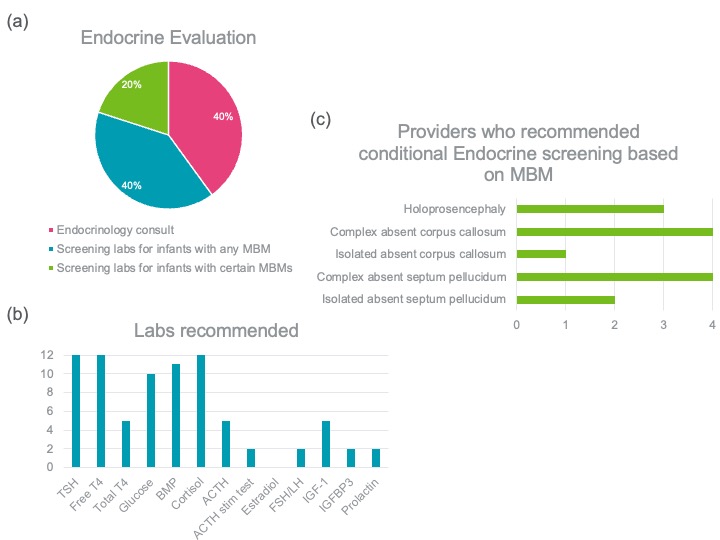 (a) While 20/20 (100%) of providers recommend endocrine screening for patients with MBMs, the pie chart shows the percentage of providers who recommend each screening method. (b) 12/20 (60%) of providers recommend specific screening labs themselves, and the blue bar graph shows the number of providers who recommend each screening lab. (c) 4/20 (20%) of providers recommend endocrine screening conditionally, for patients with certain MBMs. The green bar graph shows the number of providers who recommend endocrine screening by MBM type.
(a) While 20/20 (100%) of providers recommend endocrine screening for patients with MBMs, the pie chart shows the percentage of providers who recommend each screening method. (b) 12/20 (60%) of providers recommend specific screening labs themselves, and the blue bar graph shows the number of providers who recommend each screening lab. (c) 4/20 (20%) of providers recommend endocrine screening conditionally, for patients with certain MBMs. The green bar graph shows the number of providers who recommend endocrine screening by MBM type. Ophthalmologic evaluation recommended for patients with MBMs.
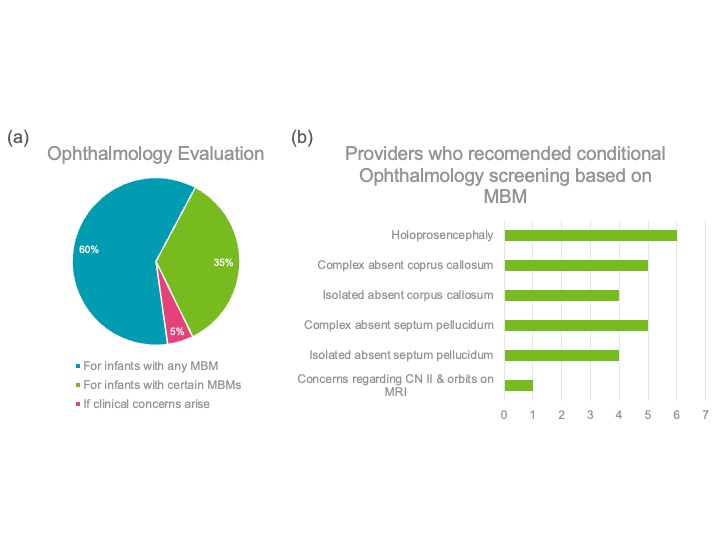 (a) The pie chart shows that while 19/20 (95%) providers recommend ophthalmology evaluation for at least some infants with MBMs, 12/20 (60%) recommend screening for infants with any MBM, and 7/20 (35%) recommend screening for infants with certain MBMs. 1/20 (5%) recommends ophthalmology evaluation only if clinical concerns arise. (b) The bar graph reveals the number of providers who recommend conditional ophthalmology screening based on the MBM.
(a) The pie chart shows that while 19/20 (95%) providers recommend ophthalmology evaluation for at least some infants with MBMs, 12/20 (60%) recommend screening for infants with any MBM, and 7/20 (35%) recommend screening for infants with certain MBMs. 1/20 (5%) recommends ophthalmology evaluation only if clinical concerns arise. (b) The bar graph reveals the number of providers who recommend conditional ophthalmology screening based on the MBM.
