Neonatal Neurology 4
Session: Neonatal Neurology 4
654 - Dynamic Multimodal Neuromonitoring for Predicting Neurodevelopmental Outcomes in Neonatal Hypoxic Ischemic Encephalopathy
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 654.4648
Srinivas Kota, University of Texas Southwestern Medical School, Dallas, TX, United States; Lynn Bitar, University of Texas Southwestern Medical School, Dallas, TX, United States; Yu-Lun Liu, University of Texas Southwestern Medical School, Dallas, TX, United States; Lina Chalak, UTSW, Dallas, TX, United States

Srinivas Kota, PhD (he/him/his)
Assistant Professor
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Neonatal Hypoxic-ischemic encephalopathy (HIE) is one of the leading causes of death or disability. While much of the existing research has focused on neuromonitoring biomarkers from a single modality to predict neurodevelopmental impairment (NDI) at two years of age, there is a significant gap in the literature regarding the use of multimodal physiological signal biomarkers to enhance predictive accuracy.
Objective: To establish quantitative neuromonitoring biomarkers on the first day of life that can predict NDI. We hypothesize that combining multimodal physiological signal biomarkers will improve the predictive accuracy for NDI.
Design/Methods: This prospective cohort study, approved by the IRB, enrolled newborns (≥36 weeks') at Parkland Hospital in Dallas, TX. A modified Sarnat examination was performed to determine the severity of HIE within the first six hours of life, and the Total Sarnat Score (TSS) was calculated. Newborns with moderate and severe HIE received therapeutic hypothermia (TH), while those with mild HIE did not undergo TH. Biomarkers including electroencephalogram (EEG) delta power (DP, 0.5 to 4 Hz) and neurovascular coupling (NVC), calculated as wavelet coherence between amplitude-integrated EEG and cerebral tissue oxygen saturation (SctO2), were measured. NDI was defined as death or a cognitive score < 85 on the Bayley Scales of Infant and Toddler Development. The predictive ability of individual biomarkers (TSS, DP, NVC) and their combination for NDI was evaluated using receiver operating characteristic (ROC) curves, with the area under the ROC curve (AUC) indicating prediction accuracy.
Results: Forty-six newborns with mild to severe HIE were enrolled (Table 1) in this NIH-funded study (NS102617). Eight out of 46 infants were lost to follow-up, and 18 (6 mild, 10 moderate, 2 severe died) had NDI. Figure 1 shows the AUC and ROC results for NDI using individual and combined biomarkers (TSS, DP, NVC). Combined biomarkers, particularly TSS with DP and NVC, demonstrated the highest predictive performance for NDI with an AUC of 0.755, sensitivity (0.750) and specificity (0.769) outperforming individual biomarkers.
Conclusion(s): This study emphasizes the importance of implementing multimodal neuromonitoring and integrating quantitative biomarkers at the bedside during the first day of life to provide objective metrics on brain health in addition to neurological exam. These approaches improve the accuracy of predicting encephalopathy severity, brain injury, and NDI, aiding clinicians in timely and effective decision-making for neuroprotective interventions.
Figure 1
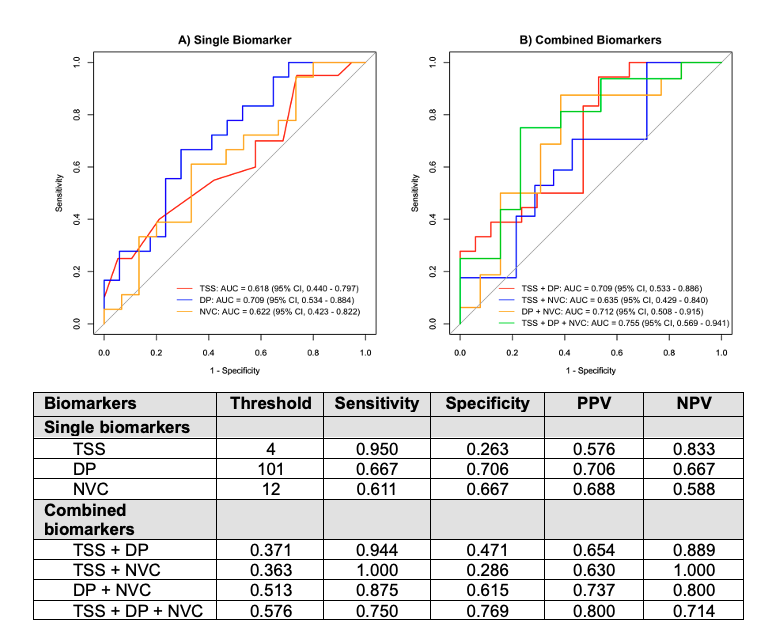 Figure 1. Receiver Operating Characteristic (ROC) Curves for Neurodevelopmental Impairment (NDI): Single Biomarker (A) and Combined Biomarkers (B). The Total Sarnat Score (TSS) was calculated using the modified Sarnat exam within the first six hours of life. EEG delta power (DP) was calculated at the cross-cerebral parietal electrodes (P3-P4). Neurovascular coupling (NVC) was calculated using wavelet coherence between amplitude-integrated EEG from central region electrodes (C3-C4) and cerebral tissue oxygen saturation (SctO2). The gray diagonal line represents the line of non-significance.
Figure 1. Receiver Operating Characteristic (ROC) Curves for Neurodevelopmental Impairment (NDI): Single Biomarker (A) and Combined Biomarkers (B). The Total Sarnat Score (TSS) was calculated using the modified Sarnat exam within the first six hours of life. EEG delta power (DP) was calculated at the cross-cerebral parietal electrodes (P3-P4). Neurovascular coupling (NVC) was calculated using wavelet coherence between amplitude-integrated EEG from central region electrodes (C3-C4) and cerebral tissue oxygen saturation (SctO2). The gray diagonal line represents the line of non-significance.Table 1
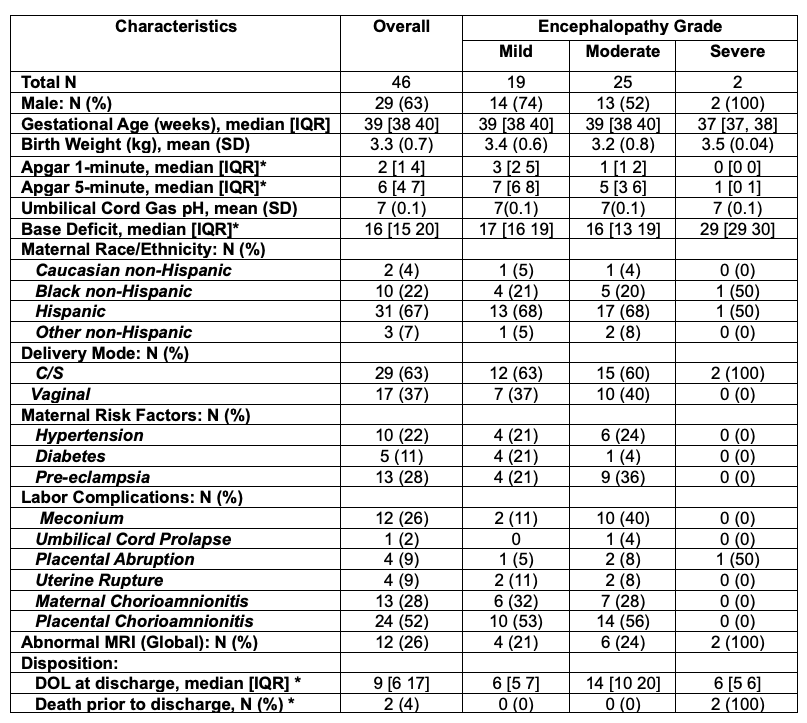 Abbreviations: DOL = days of life
Abbreviations: DOL = days of lifeThe normality of continuous variables was assessed using the Shapiro-Wilk test. Continuous Variables with a normal distribution were reported as mean with standard deviation (SD), and group comparisons were made using a one-way analysis of variance (ANOVA). For non-normally distributed continuous variables, data were presented as median with interquartile range (IQR), and comparisons were conducted using the Kruskal-Wallis test. Categorical variables were expressed as counts and percentages, and χ^2 or Fisher’s exact test was applied for comparison. Statistical significance was defined as a two-sided P value of less than 0.05.
* Indicates statistical significance (p < 0.05)
Figure 1
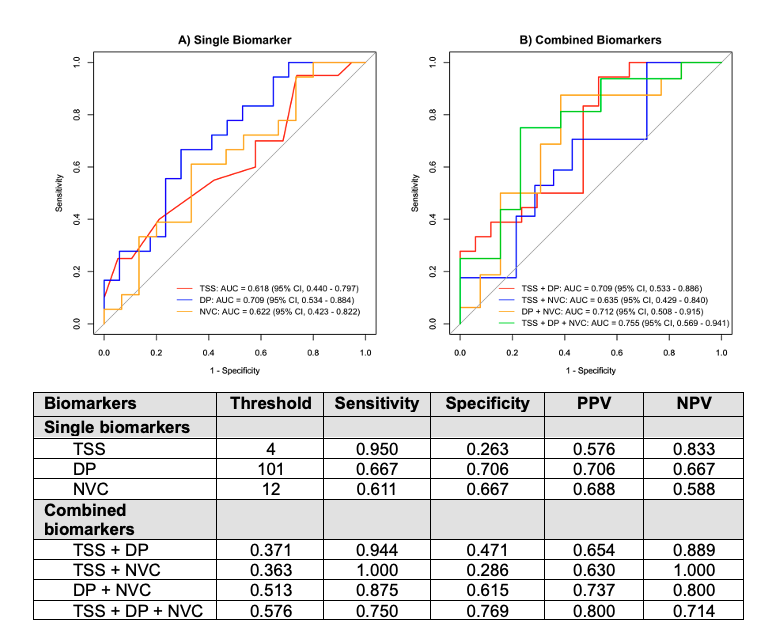 Figure 1. Receiver Operating Characteristic (ROC) Curves for Neurodevelopmental Impairment (NDI): Single Biomarker (A) and Combined Biomarkers (B). The Total Sarnat Score (TSS) was calculated using the modified Sarnat exam within the first six hours of life. EEG delta power (DP) was calculated at the cross-cerebral parietal electrodes (P3-P4). Neurovascular coupling (NVC) was calculated using wavelet coherence between amplitude-integrated EEG from central region electrodes (C3-C4) and cerebral tissue oxygen saturation (SctO2). The gray diagonal line represents the line of non-significance.
Figure 1. Receiver Operating Characteristic (ROC) Curves for Neurodevelopmental Impairment (NDI): Single Biomarker (A) and Combined Biomarkers (B). The Total Sarnat Score (TSS) was calculated using the modified Sarnat exam within the first six hours of life. EEG delta power (DP) was calculated at the cross-cerebral parietal electrodes (P3-P4). Neurovascular coupling (NVC) was calculated using wavelet coherence between amplitude-integrated EEG from central region electrodes (C3-C4) and cerebral tissue oxygen saturation (SctO2). The gray diagonal line represents the line of non-significance.Table 1
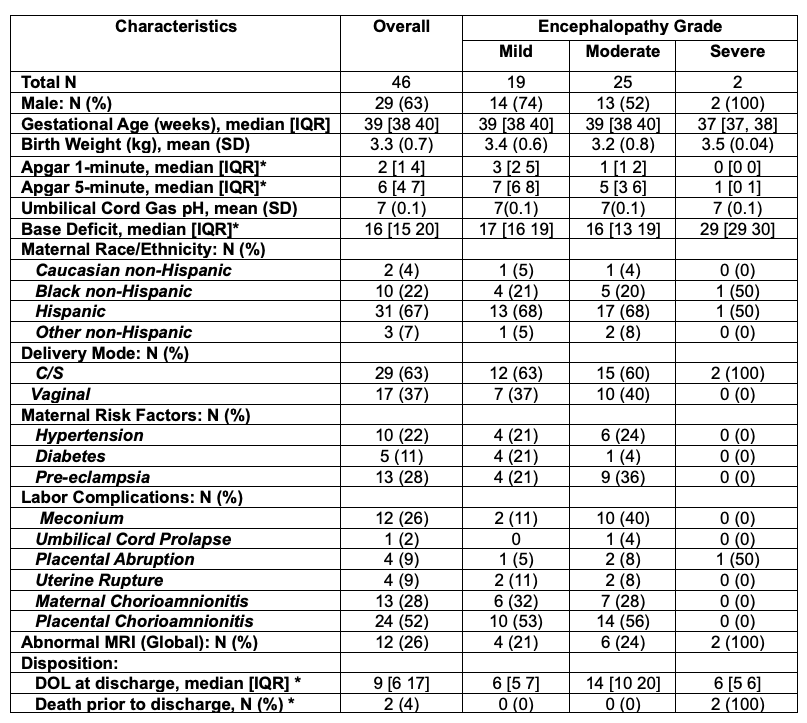 Abbreviations: DOL = days of life
Abbreviations: DOL = days of lifeThe normality of continuous variables was assessed using the Shapiro-Wilk test. Continuous Variables with a normal distribution were reported as mean with standard deviation (SD), and group comparisons were made using a one-way analysis of variance (ANOVA). For non-normally distributed continuous variables, data were presented as median with interquartile range (IQR), and comparisons were conducted using the Kruskal-Wallis test. Categorical variables were expressed as counts and percentages, and χ^2 or Fisher’s exact test was applied for comparison. Statistical significance was defined as a two-sided P value of less than 0.05.
* Indicates statistical significance (p < 0.05)

