Nephrology 2
Session: Nephrology 2
023 - Kidney Scarring in Single versus Recurrent Urinary Tract Infection in Refluxing Mice
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 23.5841
Evan A. Rajadhyaksha, Riley Hospital for Children at Indiana University Health, Indianapolis, IN, United States; Vijay Saxena, Indiana University School of Medicine, Indianapolis, IN, United States; Samuel Arregui, Indiana University School of Medicine, Indianapolis, IN, United States; Andrew Schwaderer, Indiana University, Indianapolis, IN, United States

Evan A. Rajadhyaksha, MD (he/him/his)
Fellow
Riley Hospital for Children at Indiana University Health
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Children with vesicoureteral reflux (VUR) are prone to recurrent episodes of pyelonephritis. Febrile urinary tract infection (UTI) has been reported to cause detectable scarring defects in 10-15% of children, characterized by focal defects on dimercaptosuccinic acid (DMSA) scan 6 months after infection. A recent analysis of kidney function in children with VUR identified that UTI episodes were associated with a decrease in eGFR without associated scarring on DMSA scans and this change was limited in the group on antibiotic prophylaxis. DMSA, previously recognized as the gold standard for scar identification, may underestimate renal damage in children with UTI and VUR.
Objective: Use a refluxing mouse model to compare the prevalence and severity of kidney scarring following infection with uropathogenic E. coli in single versus recurrent UTI.
Design/Methods: 40 female C3H/HeOuJ mice with vesicoureteral reflux were obtained from Jackson River laboratory. 15 were given a single UTI with uropathogenic E. coli (UPEC), and 15 were given four UTI with UPEC, inoculations each 7 days apart. All infected mice were treated with intraperitoneal cefpirome starting at 48 hours to mirror frequent clinical presentation on day 2 of illness. 10 mice served as noninfected controls. All mice were sacrificed 4 weeks after their final UPEC inoculation. Transcutaneous glomerular filtration rate (tGFR) was measured in 15 mice to establish a baseline, using FTC-labeled sinestrin and MediBeacon transcutaneous devices. Post-intervention tGFR was performed for all mice within 5 days of euthanasia. Renal fibrosis scoring system for Masson’s trichrome was scaled 0-5 (0 = no blue staining, 1 = < 10%, 2 = 10-20%, 3 = 20-40%, 4 = 40-60%, 5= >60%). Grading of 1 constituted mild, 2-3 moderate, and 4-5 severe scarring.
Results: Of the single UTI group, 13/15 mice had moderate or severe scarring on Masson’s trichrome stain. Of the recurrent UTI group, 15/15 had moderate or severe scarring on Masson’s trichrome stain. Fibrosis severity score was elevated from baseline in both infected groups, but not in uninfected controls (Figure 1). Representative scarring (25th and 75th percentile severity for each group) are shown (Figure 2).
Conclusion(s): A mouse model of VUR and UTI resulted in histologic scarring after even a single UTI. There was a significant component of diffuse interstitial collagen deposition, which differs from the classic segmental scars seen on DMSA. Evaluating this in conjunction with recent retrospective evaluation of GFR in the RIVUR cohort, we may be underestimating clinically relevant kidney scarring in children with VUR.
Figure 1. Kidney Fibrosis Score on Masson Trichome versus Intervention Group Number of UTI Episodes.
.jpg) Kruskal-Wallis test revealed a significant difference between groups, comparing ranks (p=0.0005). Means with standard deviation are plotted. Post-hoc Dunn’s multiple comparison p values are denoted between groups.
Kruskal-Wallis test revealed a significant difference between groups, comparing ranks (p=0.0005). Means with standard deviation are plotted. Post-hoc Dunn’s multiple comparison p values are denoted between groups.Figure 2. Scarring profiles.
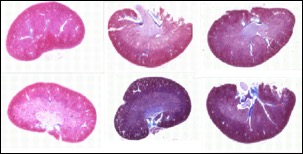 Representative scarring profiles (Masson’s trichrome), displaying 25th and 75th percentile scars for each group.
Representative scarring profiles (Masson’s trichrome), displaying 25th and 75th percentile scars for each group.
