Neonatal Clinical Trials 2
Session: Neonatal Clinical Trials 2
571 - Familial and Genetic Susceptibility to Necrotizing Enterocolitis and Spontaneous Intestinal Perforation in the Very Premature Twins: a twin data from Chinese Neonatal Network
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 571.4867
lijuan Luo, the Affiliated Hospital of Southwest Medical University, Luzhou, Sichuan, China (People's Republic); Wenbin Dong, Advocate Children's Hospital - Park Ridge, Luzhou, Sichuan, China (People's Republic); Jie Yang, Fudan Children's Hospital, Shanghai, Shanghai, China (People's Republic); Xiaoping Lei, AFFILIATED HOSPITAL OF SOUTHWEST MEDICAL UNIVERSITY, Luzhou, Sichuan, China (People's Republic)

lijuan Luo (she/her/hers)
Attending physician
the Affiliated Hospital of Southwest Medical University
Luzhou, Sichuan, China (People's Republic)
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) and spontaneous intestinal perforation (SIP) are the most devastating gastrointestinal diseases of very preterm infants, and there might be a familial (genetic and shared environmental factors) and genetic susceptibility for the development of NEC and SIP.
Objective: To demonstrate the familial and genetic susceptibility to NEC and SIP in very preterm twins in China.
Design/Methods: A retrospective study (2019-2022) from Chinese Neonatal Network (CHNN), it includes twin pairs born with gestational age less than 32 weeks or birth weight less than 1500g (Figure 1). Mixed-effects logistic-regression and latent variable probit model analysis were performed to assess the effect of specific covariates and the familial susceptibility to NEC and SIP in 2034 twin pairs. Genetic susceptibility was assessed by comparing the concordance rates in a subset of 1748 monozygotic and dizygotic twin pairs. A random risk factors was assessed by comparing the covariates within a subset of 188 pairs with one NEC or SIP.
Results: Finally, 2034 twin pairs were included in our study, with 234 NEC and SIP (Figure 1.). We found that blood transfusion, sepsis, antenatal steriods, catheter and vasoactive agent were significant covariates for NEC or SIP by Mixed-effects logistic-regression (Table 1.). After controlling for specific covariates, familial susceptibility accounted for 22.1% and genetic susceptibility accounted for 13.72% of the variance in liability for NEC and SIP. Blood transfusion, sepsis, long duration of antibiotics, catheter and vasoactive agent were risk factors within a subset pairs with one NEC or SIP (Table 2.).
Conclusion(s): The etiology of NEC and SIP is multifactorial, including both genetic and environmental factors. Our data suggest that familial and genetic susceptibility are less proportional. As clinicians, we need to pay more attention to individual risk factors such as blood transfusion, sepsis, long duration of antibiotics, catheter and vasoactive agent.
Figure 1. Study Flow Chart
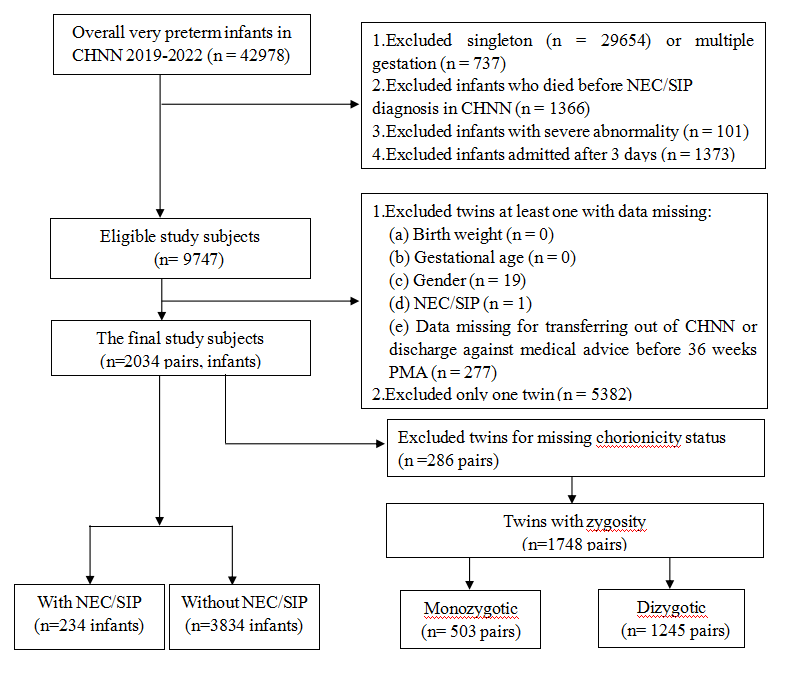
Table 1. Mixed-effects logistic-regression analysis for NEC/SIP.
Table1.pdf
Table 2. Risk factors for one infant with NEC/SIP in twins.
Table2.pdf

