Public Health & Prevention 1
Session: Public Health & Prevention 1
371 - Perspectives on WIC Referrals in DC: A Qualitative Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 371.6213
Tayler Westby, Georgetown University School of Medicine, Arlington, VA, United States; Karen Ganacias, Medstar Georgetown University Hospital, Washington, DC, United States; Janine Rethy, Georgetown University School of Medicine, WASHINGTON, DC, United States

Tayler Westby, MD Candidate, BS (they/them/theirs)
Medical Student
Georgetown University School of Medicine
Arlington, Virginia, United States
Presenting Author(s)
Background: 53% of Black and Hispanic DC residents reported acutely experiencing food insecurity compared to only 17% of their white counterparts, with 40% of these households including children. Despite the need for nutritional support, only 57.9% of those eligible for the Supplemental Nutrition Program for Women, Infants, and Children (WIC) in DC receive the benefits. An ongoing collaboration between MedStar Georgetown University Hospital Community Pediatrics, the DC AAP, and DC WIC has worked to improve communication and enrollment between pediatric providers and WIC. In the past year, an online platform for referrals was co-developed and launched to ease the process of connecting patients from healthcare providers to WIC. See Fig. 1.
Objective: This qualitative study was designed to elicit the perceptions, utilization, and barriers of key informants on the new referral platform and process.
Design/Methods: 16 semi-structured interviews were conducted with four key groups (pediatric providers, clinic social support staff, WIC staff, and WIC recipients) and conducted via Zoom between June -July 2024. Transcripts were de-identified, aggregated, and coded. Via inductive thematic analysis, six themes were identified and externally verified by 8 participants.
Results: Six themes emerged from interviews. See Table 1.
Online referral form and portal: The online portal was well accepted and utilized by most stakeholders.
Identifying eligible patients: In the clinical setting, the use of a social needs (SDOH) screening tool was essential in identifying food insecure patients and subsequently WIC eligible patients.
Perception of WIC services: Family members and providers perceive WIC as primarily offering formula and were less aware of the expansive services and resources available.
Bidirectional communication between providers and WIC staff: The online referral portal was being utilized to show the status of referrals, but providers expressed a potential benefit of WIC sharing additional clinical information such as hemoglobin results.
Enhancing enrollment: Providers and WIC staff discussed the additional benefits of co-location of WIC with providers to enhance communication and enrollment.
Key influencers for WIC enrollment: All family members interviewed discussed how their family or friends had played a role in educating and referring them to WIC.
Conclusion(s): The new online referral platform co-created with a health system and a government agency was accepted and utilized by key stakeholders and was regarded positively in modernizing communication methods though there remain opportunities for enhancements.
Table 1
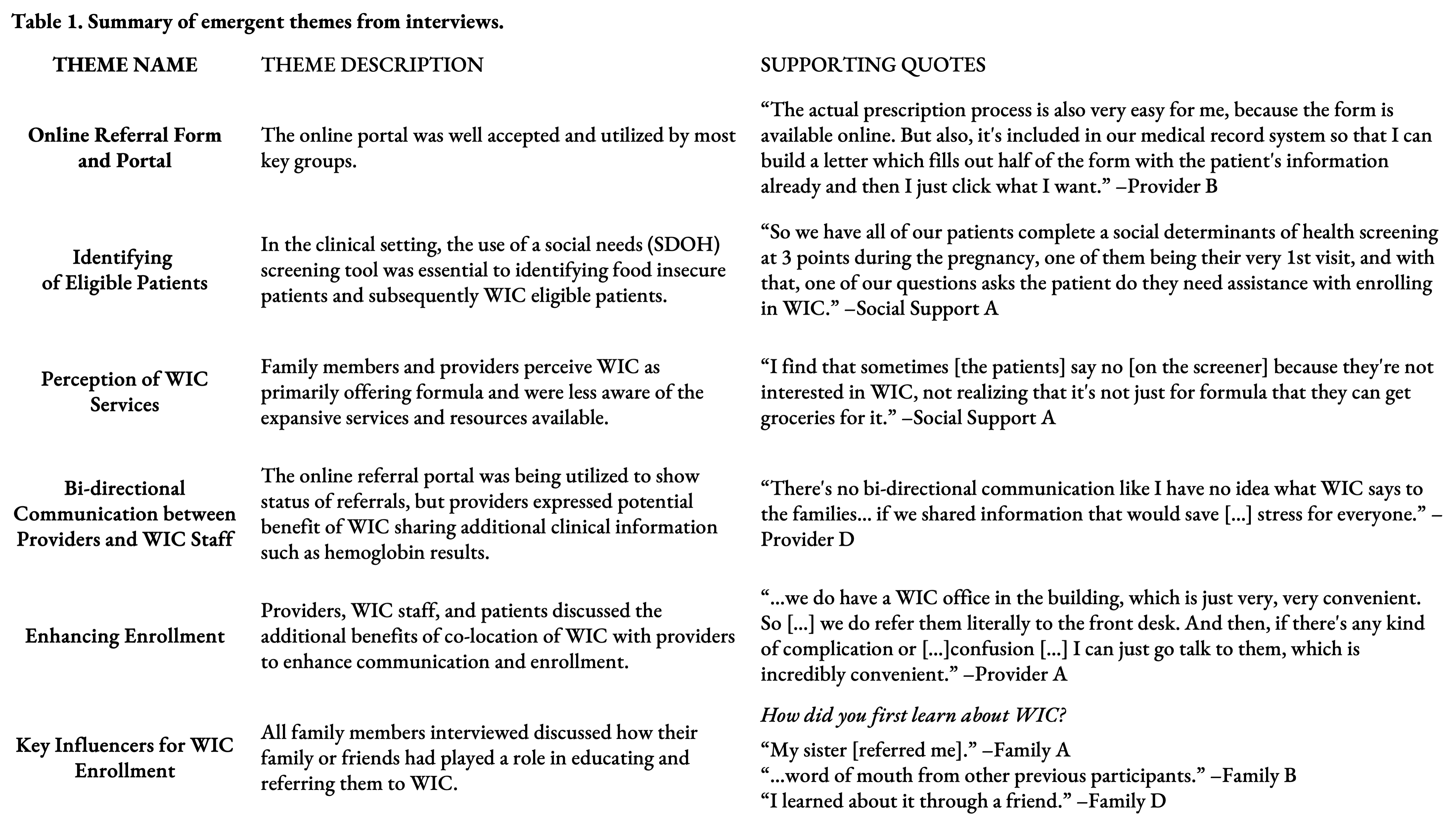 Summary of emergent themes and supporting quotes.
Summary of emergent themes and supporting quotes.Figure 1
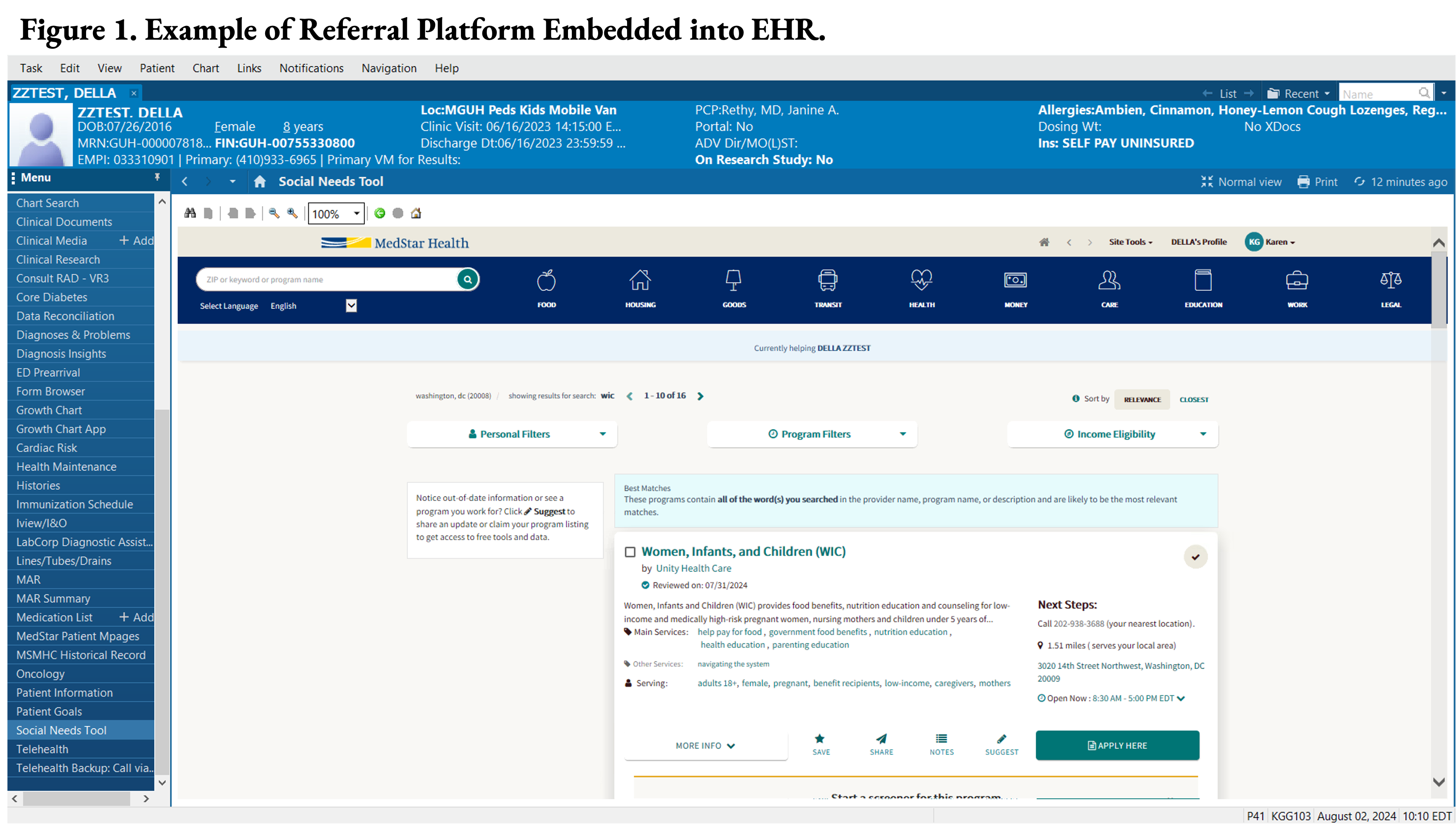 Example of WIC referral platform embedded into the EHR.
Example of WIC referral platform embedded into the EHR. Figure 2
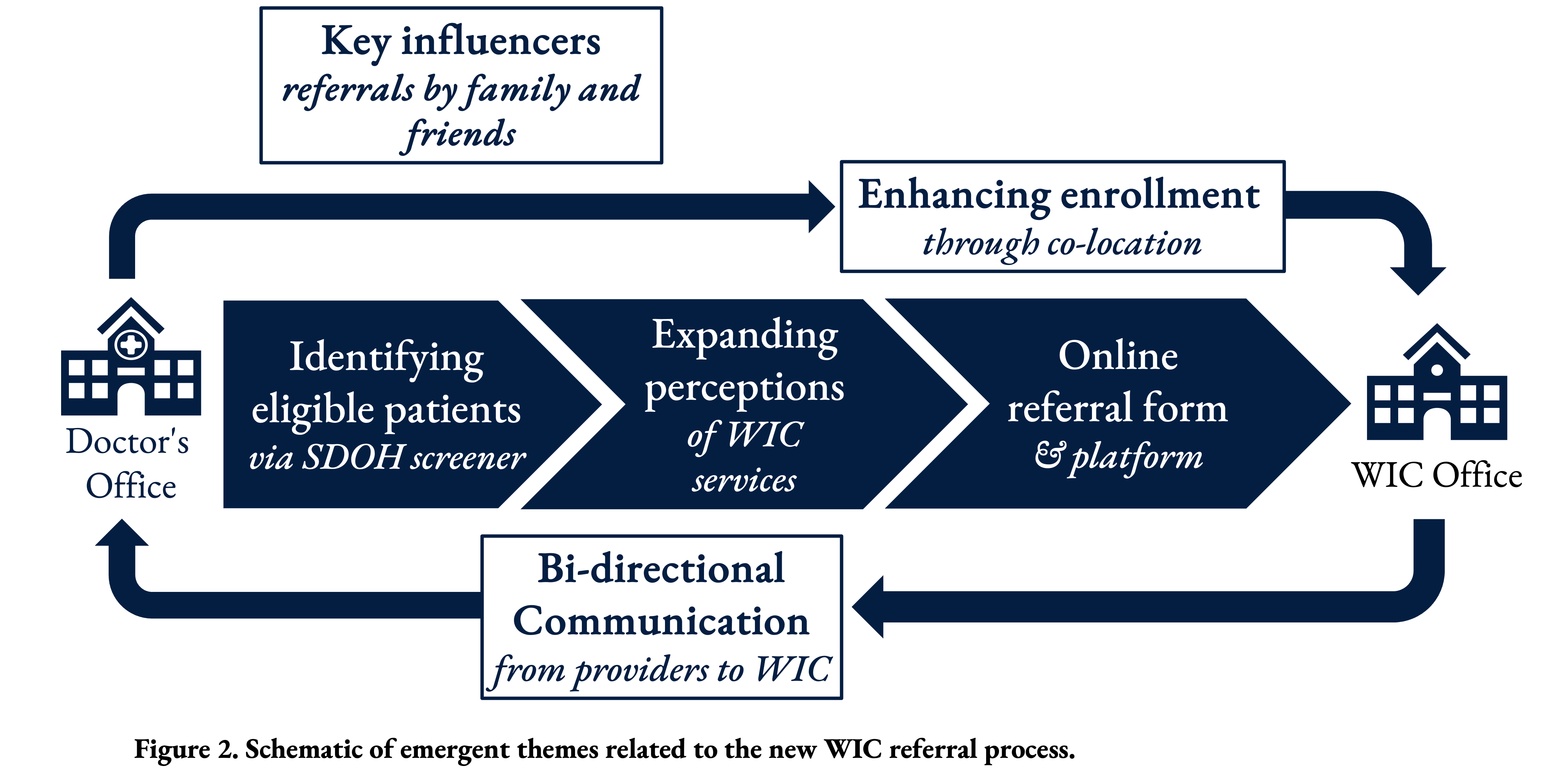 Schematic of emergent themes related to the new WIC referral process.
Schematic of emergent themes related to the new WIC referral process. 
