Neonatal Neurology 4
Session: Neonatal Neurology 4
652 - Regional Tissue Oxygenation and Feeding Outcomes in Neonates Undergoing Therapeutic Hypothermia for Hypoxic-Ischemic Encephalopathy
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 652.6434
Daniel Diatlov, Stanford University School of Medicine, Stanford, CA, United States; Olivia S.R.. Ledbury, Stanford University School of Medicine, Battle Ground, WA, United States; Valerie Y.. Chock, Stanford University School of Medicine, Sunnyvale, CA, United States

Daniel Diatlov, MSc
Medical Student
Stanford University School of Medicine
Stanford, California, United States
Presenting Author(s)
Background: Therapeutic hypothermia (TH) has been shown to improve survival and neurodevelopmental outcomes in neonates with hypoxic-ischemic encephalopathy (HIE). However, feeding outcomes in this population are poorly understood. Near-infrared spectroscopy (NIRS) is a non-invasive technology used in the neonatal intensive care unit (NICU) to monitor cerebral, renal, and mesenteric tissue oxygen saturation (CSAT, RSAT, and MSAT). These regional tissue oxygenation measures may serve as prognostic markers of feeding outcomes in neonates with HIE.
Objective: To correlate cerebral, renal, and mesenteric tissue oxygenation levels with neonatal feeding outcomes including days until any feeds, days until full volume feeds, body weight percentile at discharge, and feeding tube use at discharge in neonates undergoing TH for HIE.
Design/Methods: This retrospective, observational study collected hourly NIRS data from neonates undergoing TH for mild, moderate, and severe HIE between 2019 and 2024 at a single, quaternary-care NICU. Demographic information and feeding outcomes were obtained from patient electronic medical records. Welch’s t-test and Spearman rank correlation testing explored the association between the NIRS measures at various time points and feeding outcomes.
Results: Data were collected from 42 neonates with a mean (SD) gestational age of 39.6 (1.3) weeks (Table 1). Mean MSAT and RSAT were lower than CSAT during cooling, but followed similar trajectories. After rewarming, mean RSAT stabilized at higher levels than MSAT or CSAT (Figure 1). Higher CSAT values were correlated with increased days until starting feeds (p=0.04 at hour 40), increased days until reaching full volume feeds (p=0.03 at hour 96), and decreased body weight percentile at discharge (p=0.04 at hour 12). Higher CSAT values at 24 hours were also associated with the need for tube feeding at discharge (p=0.0002) (Figure 2). No significant correlations were found between feeding outcomes and MSAT or RSAT data.
Conclusion(s): MSAT did not significantly correlate with neonatal feeding outcomes. However, higher CSAT levels may be associated with adverse feeding outcomes, suggesting those with normal CSAT values may start feeds earlier and be discharged at a greater weight percentile. Future large targeted studies may better distinguish the relationship between NIRS monitoring and feeding outcomes in neonates undergoing TH for HIE.
Table 1. Study cohort characteristics.
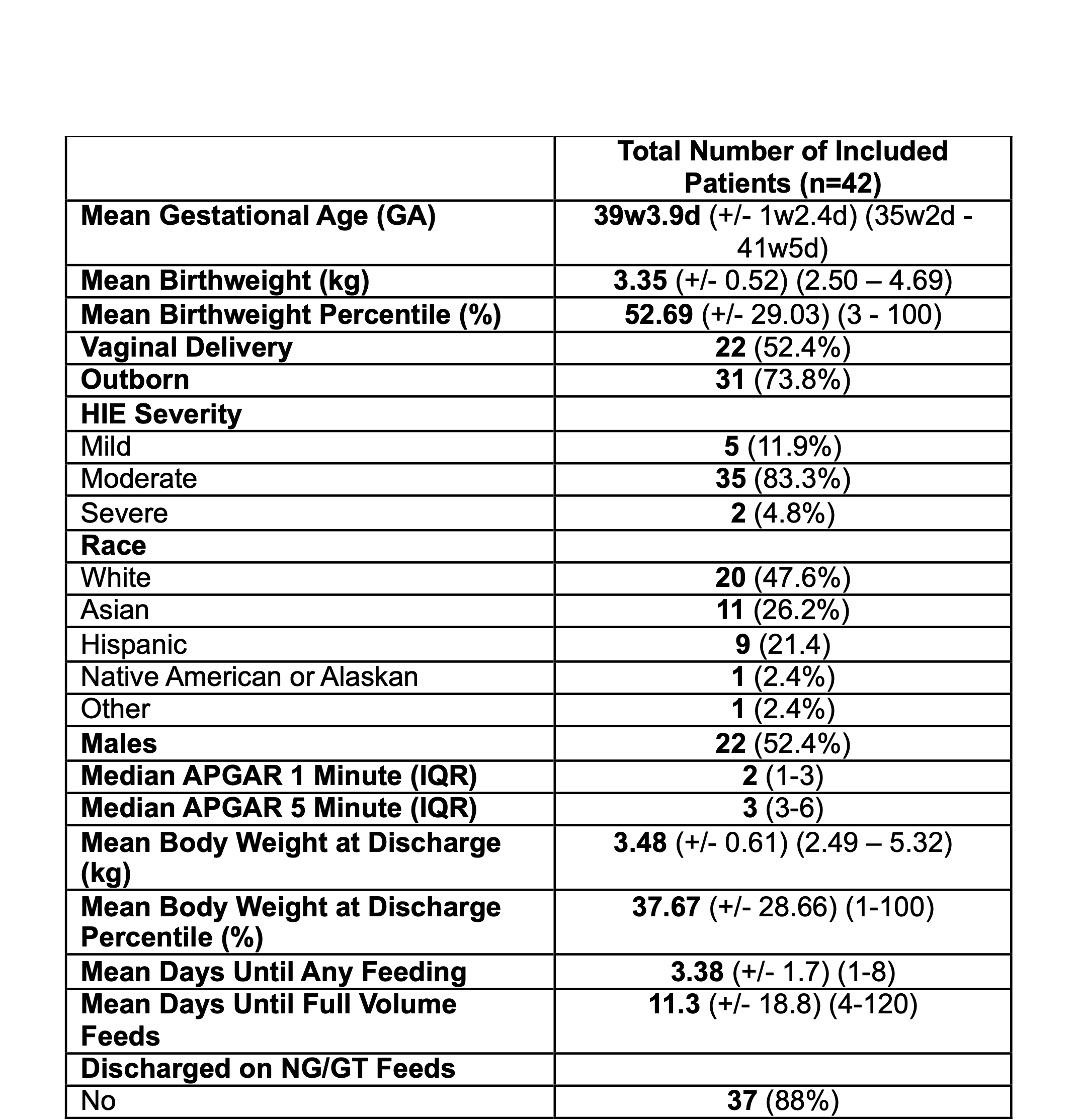
Figure 1. Mean hourly CSAT, RSAT, and MSAT values from hour-of-life (HOL) 6 to 120.
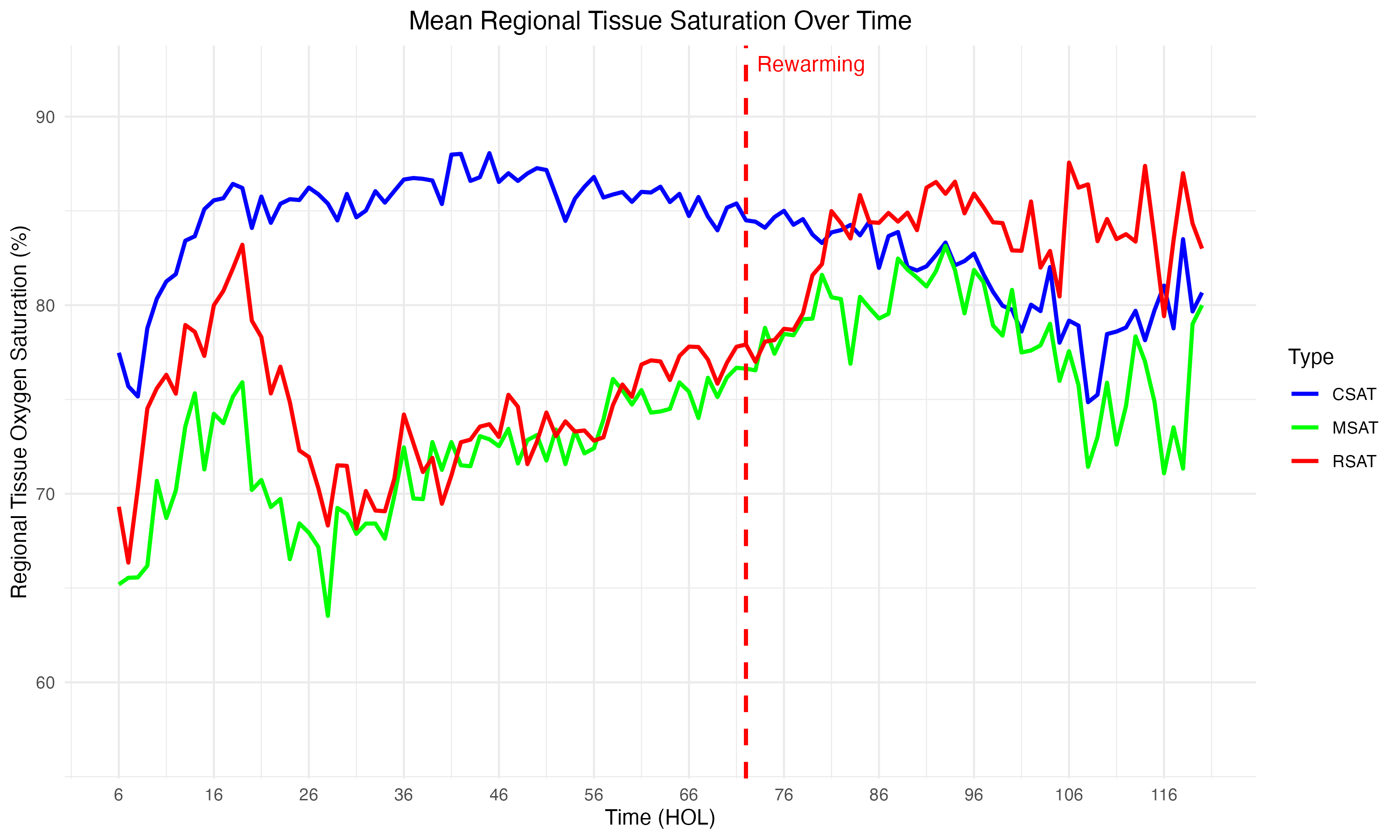
Figure 2. Associations between NIRS measures at various timepoints and feeding outcomes.
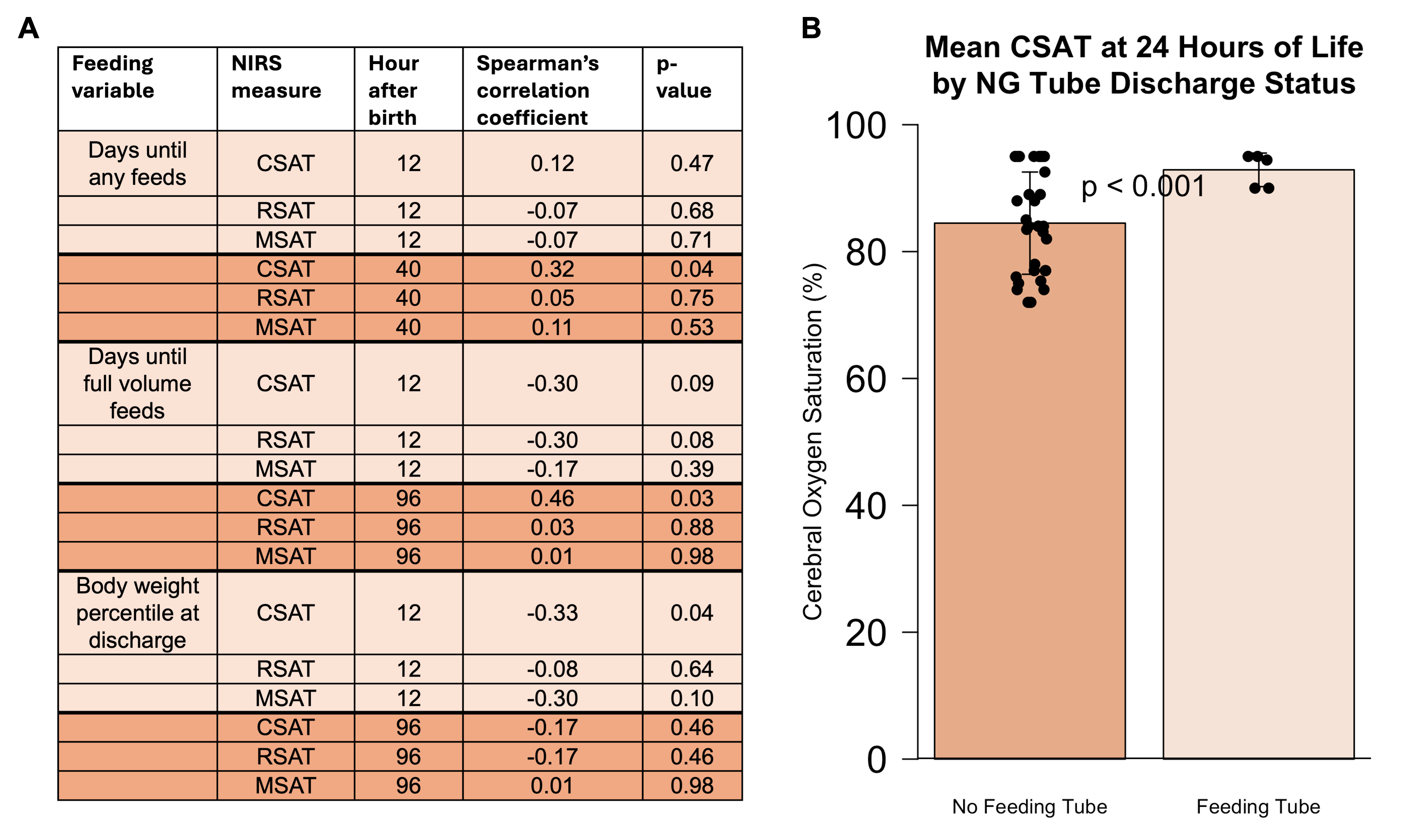 (A) Summary of correlations between feeding outcomes and NIRS measures at early and late time points. (B) Association between CSAT value and feeding tube discharge status at 24 hours of life (p=0.0002).
(A) Summary of correlations between feeding outcomes and NIRS measures at early and late time points. (B) Association between CSAT value and feeding tube discharge status at 24 hours of life (p=0.0002). 
