Neonatal Neurology 6: Neurodevelopment
Session: Neonatal Neurology 6: Neurodevelopment
682 - Predictive Ability of the Hammersmith Neonatal Neurological Examination for Identifying Neurodevelopmental Impairment in High-Risk Infants at 2 Years Corrected Age
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 682.6329
Jiarui Liu, Duke-NUS Medical School, Singapore, N/A, Singapore; Imelda Lustestica. Ereno, Singapore General Hospital, Singapore, N/A, Singapore; Vijay Baral, SingHealth Services, Singapore, N/A, Singapore; Kelly Ann Zainal, Singapore General Hospital, Singapore, N/A, Singapore; Jaslyn Ong, Singapore General Hospital, Singapore, N/A, Singapore; Jing Shi Chua, Singapore General Hospital, Singapore, N/A, Singapore; Joo Guan Yeo, KK Women's and Children's Hospital, Singapore, N/A, Singapore; Cheo Lian Yeo, Singapore General Hospital, Singapore, N/A, Singapore
- JL
Jiarui Liu, BSc (she/her/hers)
Student
Duke-NUS Medical School
Singapore, Singapore
Presenting Author(s)
Background: Early preterm and small-for-gestational-age infants face an increased risk of neurodevelopmental impairment, underscoring the need for early identification to facilitate timely interventions. The Hammersmith Neonatal Neurological Examination (HNNE) is widely used to assess early neurological function in newborns, but its long-term predictive value for developmental risks remains underexplored. We hypothesize that the HNNE done at term corrected age (TCA) can identify those with eventual motor, cognitive, or language impairment.
Objective: We aim to evaluate the predictive ability of the HNNE at TCA in forecasting motor, cognitive, and language impairments at 2 years corrected age (CA).
Design/Methods: We evaluated 90 infants born at less than 32 weeks’ gestation and/or weighing less than 1250 grams at Singapore General Hospital, all of whom underwent the HNNE at TCA of 37-41 weeks. HNNE scores were categorized as optimal vs. sub-optimal based on cut-off scores derived from a predominantly Asian cohort of preterm infants. The primary outcome was measured at 2 years CA using the Bayley Scales of Infant and Toddler Development (BSID), Third and Fourth Editions. BSID composite scores were classified as non-critical vs. critical impairment based on established cut-off scores for Motor, Cognitive, and Language domains. Sensitivity analysis and Receiver Operating Characteristic (ROC) curves were employed to evaluate the predictive ability of sub-optimal HNNE scores in determining critical neurodevelopmental impairment.
Results: The HNNE at TCA demonstrated greater sensitivity and specificity in predicting critical motor impairments compared to cognitive or language impairments, with sensitivities of 75.0%, 66.7%, and 44.4%, and specificities of 64.5%, 61.9%, and 63%, respectively. The AUC for predicting critical motor impairment was 0.803 (p = 0.042), while AUCs for cognitive and language impairments were 0.726 (p = 0.185) and 0.623 (p = 0.232), respectively .
Conclusion(s): The HNNE at TCA can effectively predict critical motor impairment at 2 years CA in early preterm infants, though it’s predictive ability for cognitive and language impairments is limited. Its ability to identify motor risk will guide early developmental interventions to optimize functional outcomes. Future research should integrate the HNNE with additional diagnostic tools that target cognitive and language risks to enhance predictive accuracy.
Figure 1
.jpg) Study population with the HNNE at TCA and BSID at 2 years CA .
Study population with the HNNE at TCA and BSID at 2 years CA . Table 1
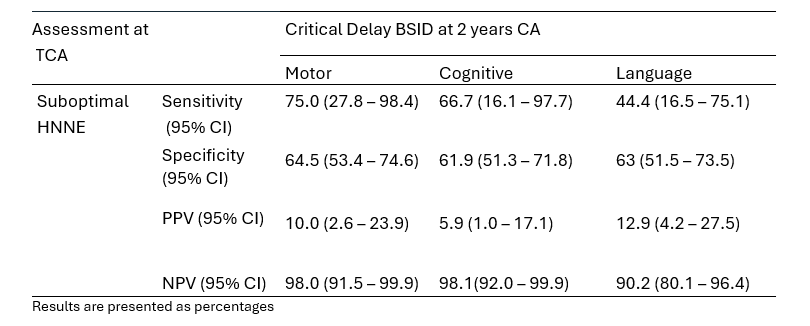 Diagnostic accuracy of HNNE at TCA for critical neurodevelopmental impairment at 2 years CA (as measured by BSID, Third & Fourth Editions).
Diagnostic accuracy of HNNE at TCA for critical neurodevelopmental impairment at 2 years CA (as measured by BSID, Third & Fourth Editions).Figure 2
.jpg) ROC curve comparing HNNE at TCA to neurodevelopmental outcomes at 2 years CA (as measured by BSID, Third & Fourth Editions), (a) Critical Motor Impairment (b) Critical Cognitive Impairment (c) Critical Language Impairment.
ROC curve comparing HNNE at TCA to neurodevelopmental outcomes at 2 years CA (as measured by BSID, Third & Fourth Editions), (a) Critical Motor Impairment (b) Critical Cognitive Impairment (c) Critical Language Impairment.
