Nephrology 1
Session: Nephrology 1
006 - Influence of Neighborhood Socioeconomic Disadvantage on Post-Kidney Transplant Obesity
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 6.5212
Bianca E. Saenz, Baylor College of Medicine, Houston, TX, United States; Elizabeth A. Onugha, Baylor College of Medicine, Houston, TX, United States; Leyat Tal, Texas Children's Hospital, Houston, TX, United States; Duc T. Nguyen, Baylor College of Medicine, Houston, TX, United States; Ankona Banerjee, Baylor College of Medicine, Houston, TX, United States; Kenneth Nobleza, Baylor College of Medicine, Houston, TX, United States; Kexin Guo, Baylor College of Medicine, Houston, TX, United States

Elizabeth A. Onugha, MD MSCI (she/her/hers)
Assistant Professor
Baylor College of Medicine
The Woodlands, Texas, United States
Presenting Author(s)
Background: Post transplantation weight (wt) gain is common in kidney transplant (KTx) recipients and increases the risk of cardiovascular (CV) disease due to the development or worsening of hypertension, dyslipidemia, new onset diabetes mellitus and obesity. Rapid wt gain in this population is influenced by various economic, psychosocial and environmental factors which can be difficult to assess.
Objective: The objective of the study is to evaluate the prevalence of obesity in the 2 years (yrs) post-transplant and examine the association of post-transplant obesity with socioeconomic factors using the area deprivation index score (ADI) in pediatric KTx recipients.
Design/Methods: A single center retrospective chart review of pediatric KTx recipients at Texas Children’s Hospital was conducted from 2014 to 2023 (n=120). Patients (pts) less than 2 yrs or more than 19 yrs at transplantation, and multi-organ or re-transplant excluded. ADI scores, a measure of neighborhood-level socioeconomic status (SES) was determined by transplant yr and home address and stratified into quartiles ranging from the least deprived neighborhoods (Q1) to the most deprived neighborhoods (Q4). Differences in pt characteristics and outcomes between groups used chi square and Fisher's exact test. Factors associated with change in BMI z-score used Kruskal Wallis test and linear mixed effect model. P-value of < 0.05 was considered statistically significant.
Results: In our cohort, 35% were obese at 2 yr follow up, compared to 13% at transplant (58.3% male, 45.8% Hispanic, median age 13 yrs at transplant). BMI z-score trend was positive in all pts and evident by 1 yr in Q1, 6 months Q2, and 1-3 months Q3-Q4. Compared to Q1, pts in Q2-Q4 were more likely to have significant increases in wt (Q2 z= 1.69, p=0.02, Q3 z=1.32, p= 0.01, Q4 z= 2.44, p= 0.02). Wt change by 2yrs significantly increased amongst all age groups (p <.001), though just BMI z-score was significant in age groups 6 yrs and older (p=0.02). We observed that residing in Q3 and being overweight or obese at transplant were significantly associated with increase in BMI z-score over time (p=0.04, p=0.02).
Conclusion(s): We found that there was a 3-fold increase in obesity prevalence at 2yr follow up with increased risk in residents of SES disadvantaged neighborhoods. Examining the influence of neighborhood-level SES disadvantage can identify pediatric KTx recipients at increased risk for CV disease and poor health outcomes. Longitudinal studies evaluating long term CV outcomes based on socioeconomic disadvantage and interventional studies mitigating these risk factors are needed.
Certification of Trainee/Education Status Bianca Saenz
Bianca fellow letter 2024.pdf
Table 1
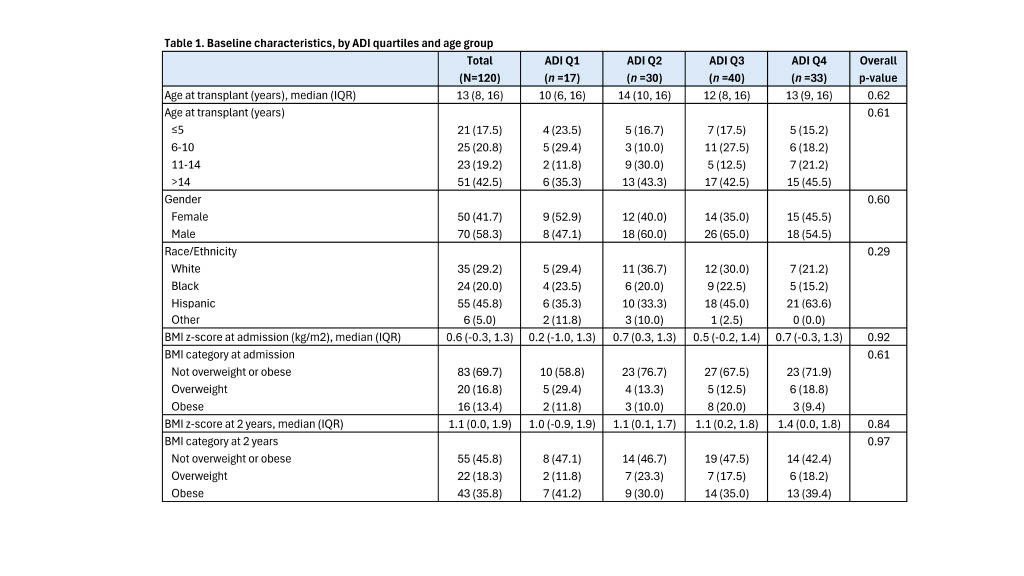 Baseline characteristics, by ADI quartiles and age group
Baseline characteristics, by ADI quartiles and age groupTable 2
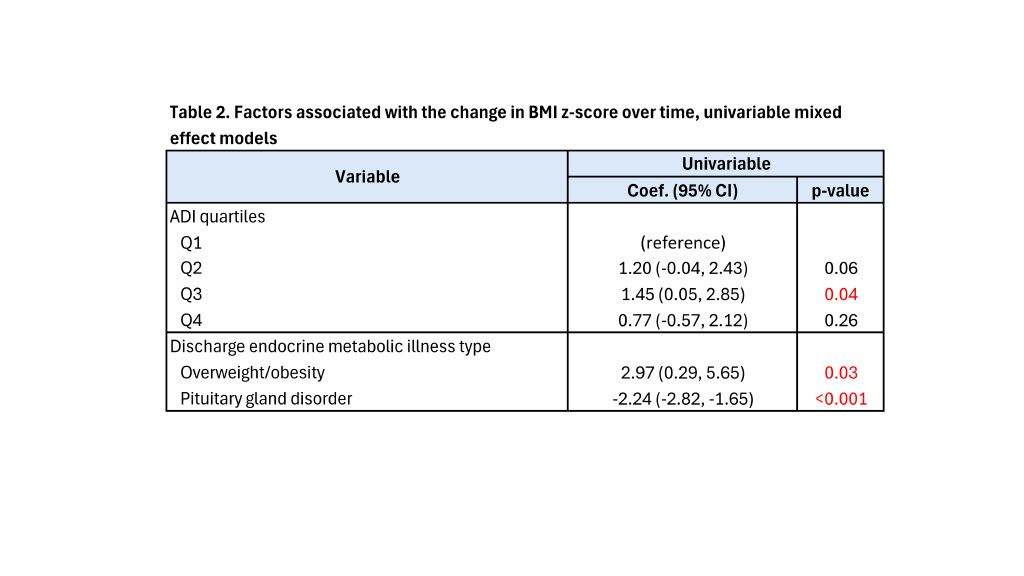 Factors associated with the change in BMI z-score over time, univariable mixed effect models
Factors associated with the change in BMI z-score over time, univariable mixed effect models
