Environmental Health 1
Session: Environmental Health 1
445 - Floods, Wildfires, Asthma, Allergies--What is the Role of the Pediatrician in Climate Action? A CORNET Survey
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 445.4797
Taryn Sirias, University of California, San Francisco, School of Medicine, Oakland, CA, United States; Jason Lau, University of Washington School of Medicine, Seattle, WA, United States; Hollyce Tyrrell, Academic Pediatric Association, McLean, VA, United States; , Yale University; Sonja M. Swenson, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Amanda Millstein, UCSF Benioff Children's Hospital Oakland, El Cerrito, CA, United States; Naomi Bardach, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Naomi S. Bardach, MD, MAS (she/her/hers)
Professor of Pediatrics and Health Policy
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Climate change poses immediate and long-term threats to child health. The American Academy of Pediatrics published a 2024 statement outlining pediatricians’ roles in climate change adaptation and mitigation, yet little is known about current pediatric trainees’ and preceptors’ climate action perceptions and practices.
Objective: To assess the capabilities, opportunities, motivation, and behaviors (COM-B) for climate action among a national sample of pediatric residents and preceptors in academic primary care centers.
Design/Methods: Using the well-established COM-B framework, we developed a survey assessing facilitators and barriers to climate-related behavior changes (“climate action”); we piloted it with practicing pediatricians and trainees in 2023. March-June 2024, we recruited site leads in the Academic Pediatric Association's Continuity Research Network (CORNET). Those who agreed to participate shared the survey with their continuity clinic residents and faculty. We analyzed data using descriptive statistics and multivariable logistic regression.
Results: There were 321 respondents from 18 sites (151 (47%) faculty; 166 (52%) residents) from all US regions (Table 1), with a 21% response rate. Most (83%) strongly agreed that climate change is happening and 46.7% strongly agreed that climate change currently affects children’s health. Respondents chose pollution (62%), allergies (54%) and heat (47%) as climate-change related issues for patients. Drought (4%) and flood (6%) were less frequent choices. 80% reported taking climate related action in the prior year (Figure 1). High priority actions included: Counseling patients and families to ameliorate the health effects of climate change (52.3%), clinic sustainability efforts (48%), and climate change advocacy (51%). Barriers were: lack of adequate knowledge and confidence (40-50%); lack of time (80-90%); low expectations of meaningful change (20-30%); lack of involved peers (17-26%); and concern about harming the family-pediatrician relationship in context of a politicized topic (20% for counseling on health effects; 25% for counseling on the connection between carbon footprint and health (Figure 2). Respondents noted that counseling patients to protect health was the action most within pediatricians’ locus of control, but that the action has low potential for addressing climate change.
Conclusion(s): In a national sample of pediatricians, lack of knowledge is an addressable capability barrier. Addressing the motivation barrier of a low sense of agency among pediatricians may promote engagement with AAP recommendations for climate action.
Table 1. Sample Respondent Characteristics (n=321)
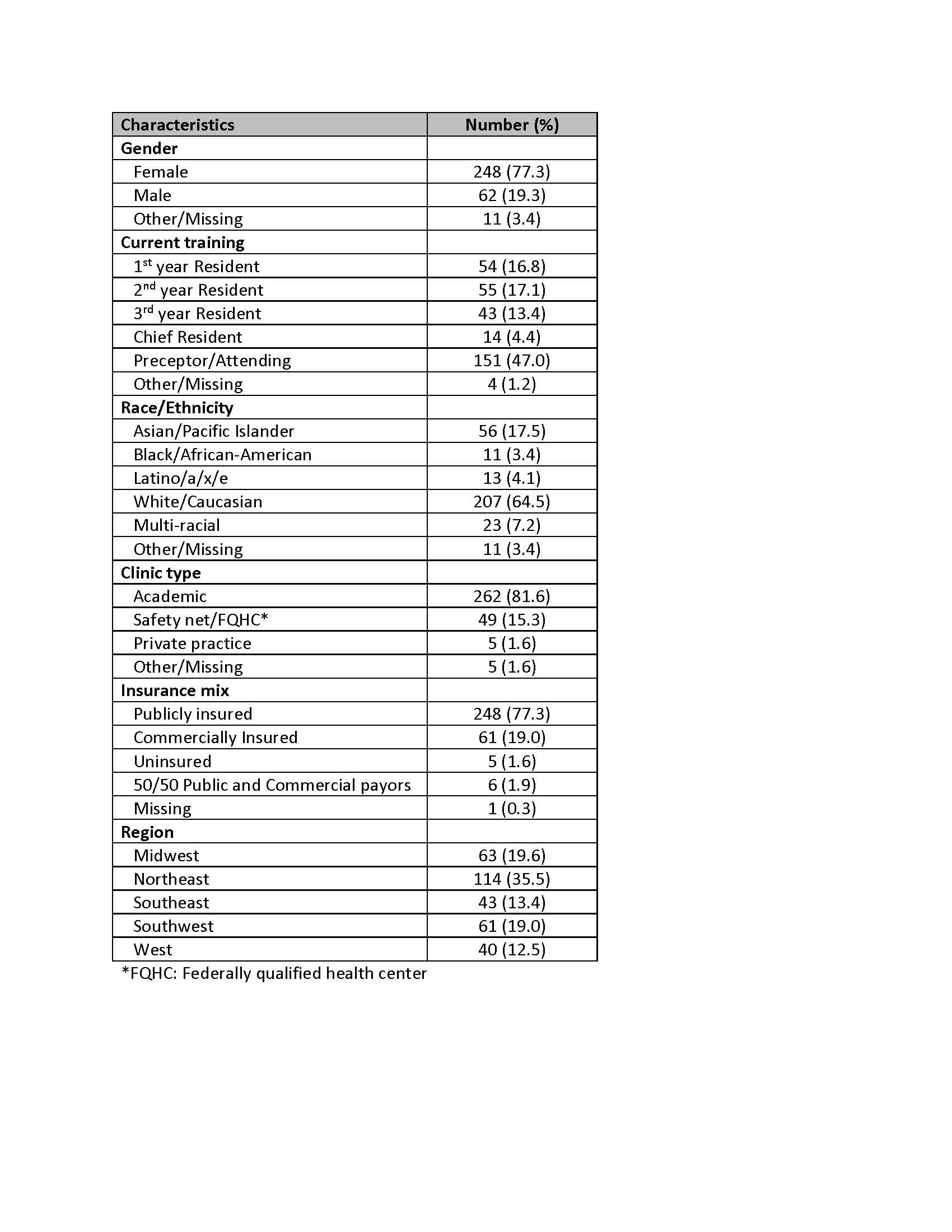
Figure 1. Climate Actions Taken in Past Year (N=321)*
.jpg) *Respondents could choose more than one response
*Respondents could choose more than one response Figure 2. Potential Climate Actions and Barriers (N=321)
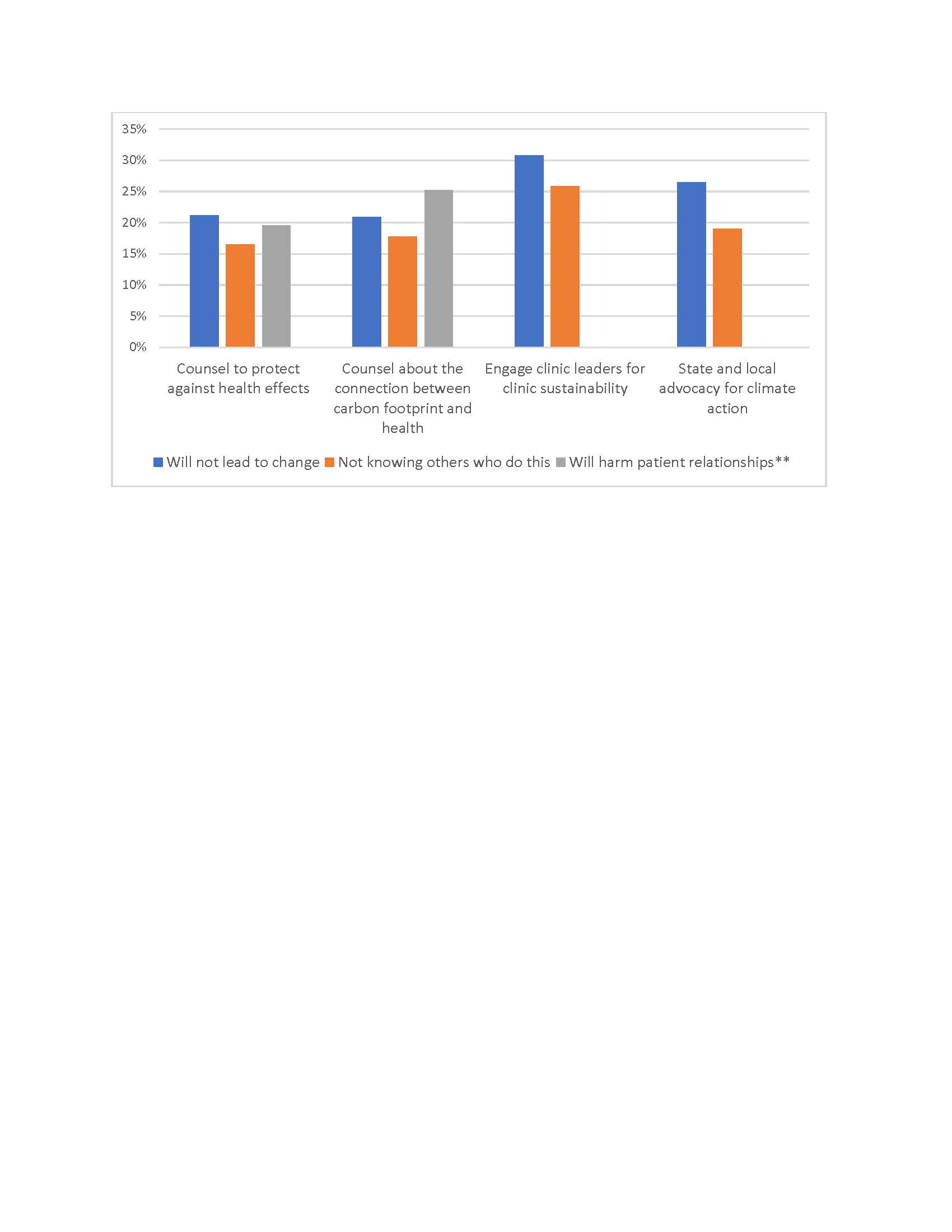 *Respondents could choose more than one response.
*Respondents could choose more than one response.**Causing harm to patient relationships was only an option for actions related to counseling patients

