Neonatal Neurology 5: Fetal
Session: Neonatal Neurology 5: Fetal
664 - Fetal Brain Volumes are Associated with Placental Pathologic Anomalies in Congenital Heart Disease: A Case-Control Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 664.4629
Claire Baldauf, Children's Hospital Los Angeles, Los Angeles, CA, United States; William Reynolds, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Valeria Rosas, Children's Hospital Los Angeles, Wilmington, CA, United States; Jodie K.. Votava-Smith, Children's Hopsital Los Angeles, Los Angeles, CA, United States; Melissa L. Wilson, USC Keck School of Medicine, Los Angeles, CA, United States; Paul Zamiara, Children's Hospital Los Angeles, Los Angeles, CA, United States; Shuo Wang, Children's Hospital Los Angeles, Los Angeles, CA, United States; Rafael Ceschin, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States; Jessica Wisnowski, Children's Hospital Los Angeles, Los Angeles, CA, United States; Vidya Rajagopalan, Children's Hospital Los Angeles, Los Angeles, CA, United States

Claire Baldauf, MD, MS (she/her/hers)
Assistant Professor
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Reduced fetal brain volume in infants with critical congenital heart disease (CHD) predicts worse neurodevelopmental outcomes. The pre-natal environment is increasingly being recognized as a critical effector. However, the role of specific placental lesions on fetal brain volume during in-utero development remains unknown.
Objective: We sought to determine the relationship between fetal brain volumes and placental pathologic anomalies in subjects with and without CHD.
Design/Methods: This was a multi-site, prospective, nested case-control study. Pregnant women with a prenatal diagnosis of fetal CHD (N=66) and those with typically developing fetuses (non-CHD, N=45) were included. Fetal brain MRI was performed between 24- and 38-weeks' gestation. Regional brain volumes were normalized to total brain volume as a ratio (i.e. regional/total volume). Total brain volume was calculated as the sum of all tissues. After delivery, placental pathology reports were reviewed and scored for six histologic features by one perinatal pathologist using the Amsterdam criteria. Heteroscedasticity robust linear regression modeling was performed in R and p< 0.05 was considered significant. Stratified examination by cohort status (CHD vs non-CHD) was also performed. Clinical maternal pregnancy risk factors were included in the model if β was changed by >10%.
Results: Placental hypoplasia, defined as placental weight < 10th %ile, was associated with lower total fetal brain volume in the combined cohort (comprising all subjects, β= -2.1 x10^4, 95% CI [-3.4 x10^4, -7.4 x10^3], p=0.002) (Figure 1). Upon stratification, subjects with CHD and placental hypoplasia had lower total brain volume than those with CHD alone (CHD, β= -2.3 x10^4, 95% CI [-4.2 x10^4, -4.9 x10^3], p=0.014). Placental hypoplasia was also associated with lower white matter volumes among CHD subjects (β= -1.17 x10^-2, 95% CI [-2.02 x10^-2, -3.23 x10^-3], p=0.008, interaction term p=0.006), but was non-significant in the non-CHD and combined cohorts. Placental vascular malperfusion (either maternal, fetal, or both) was associated with lower total fetal brain volume in the combined cohort (β= -1.7 x10^4, 95% CI [-3.3 x10^4, -5.2 x10^2], p=0.043), and in stratified analyses, the non-CHD cohort (β= -3.0 x10^4, 95% CI [-5.3 x10^4, -6.7 x10^3], p=0.013).
Conclusion(s): Placental hypoplasia and vascular malperfusion are associated with decreased total fetal brain volumes. The fetal white matter is particularly vulnerable in CHD. Specific placental pathologies differentially impact fetal brain development in the setting of CHD compared to the typically developing fetal brain.
Figure 1
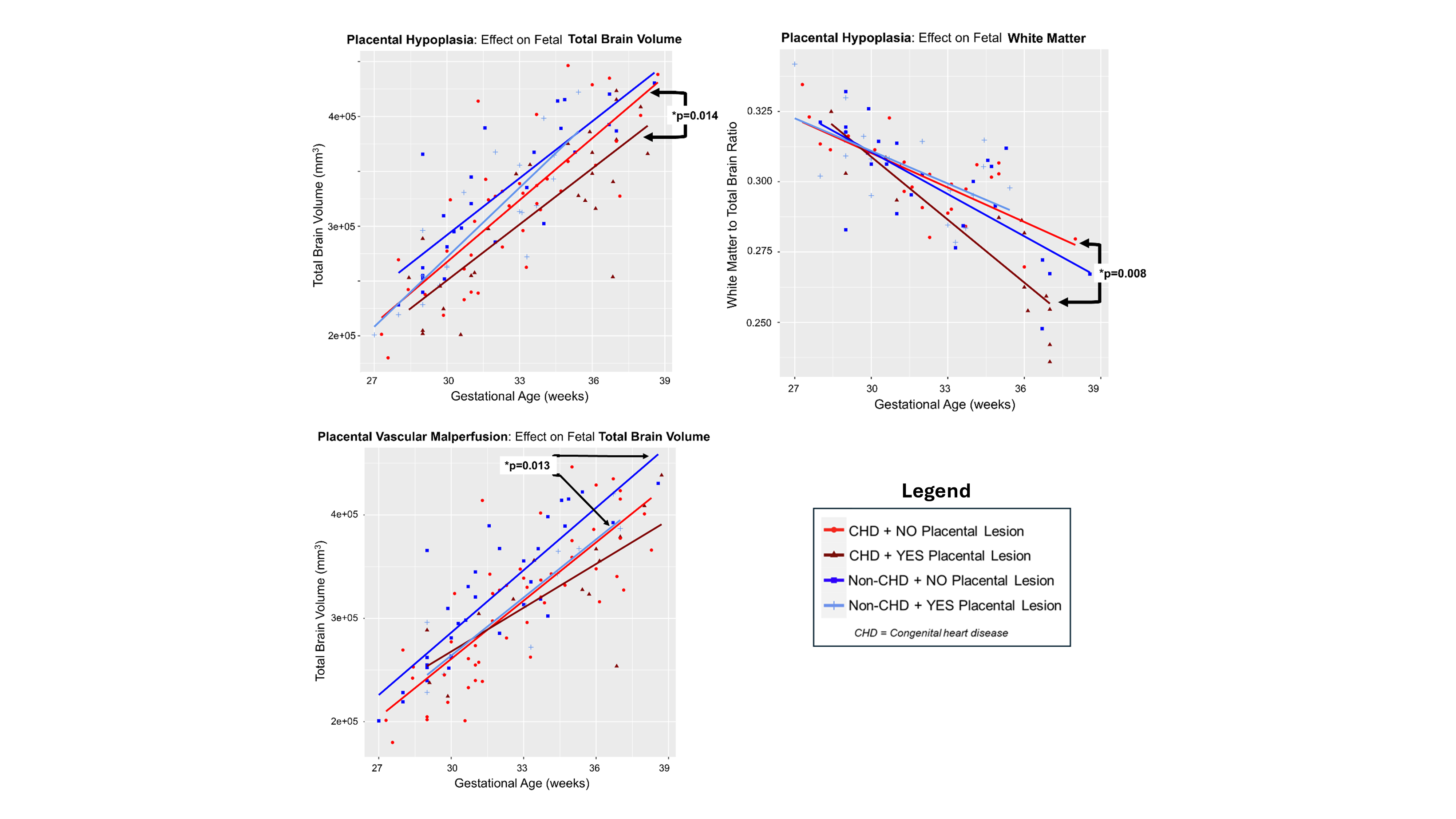 The effect of placental hypoplasia and placental vascular malperfusion on brain volume in fetuses with congenital heart disease (CHD) and those without (non-CHD). A, B) Within the CHD cohort, the presence of placental hypoplasia (defined as placental weight < 10th percentile) is associated with significantly lower total fetal brain volume (p=0.014) and reduced normalized fetal white matter volume (p=0.008). Non-CHD subjects did not show a significant difference between those with and without placental hypoplasia. C) Placental vascular malperfusion (either maternal, fetal, or both) was associated with lower total fetal brain volume in the combined cohort (inclusive of fetuses with and without CHD) (p=0.043), as well as the non-CHD cohort in stratified analysis (p=0.013). Fetuses affected by both CHD and placental vascular malperfusion demonstrated the smallest total brain volumes.
The effect of placental hypoplasia and placental vascular malperfusion on brain volume in fetuses with congenital heart disease (CHD) and those without (non-CHD). A, B) Within the CHD cohort, the presence of placental hypoplasia (defined as placental weight < 10th percentile) is associated with significantly lower total fetal brain volume (p=0.014) and reduced normalized fetal white matter volume (p=0.008). Non-CHD subjects did not show a significant difference between those with and without placental hypoplasia. C) Placental vascular malperfusion (either maternal, fetal, or both) was associated with lower total fetal brain volume in the combined cohort (inclusive of fetuses with and without CHD) (p=0.043), as well as the non-CHD cohort in stratified analysis (p=0.013). Fetuses affected by both CHD and placental vascular malperfusion demonstrated the smallest total brain volumes. Figure 1
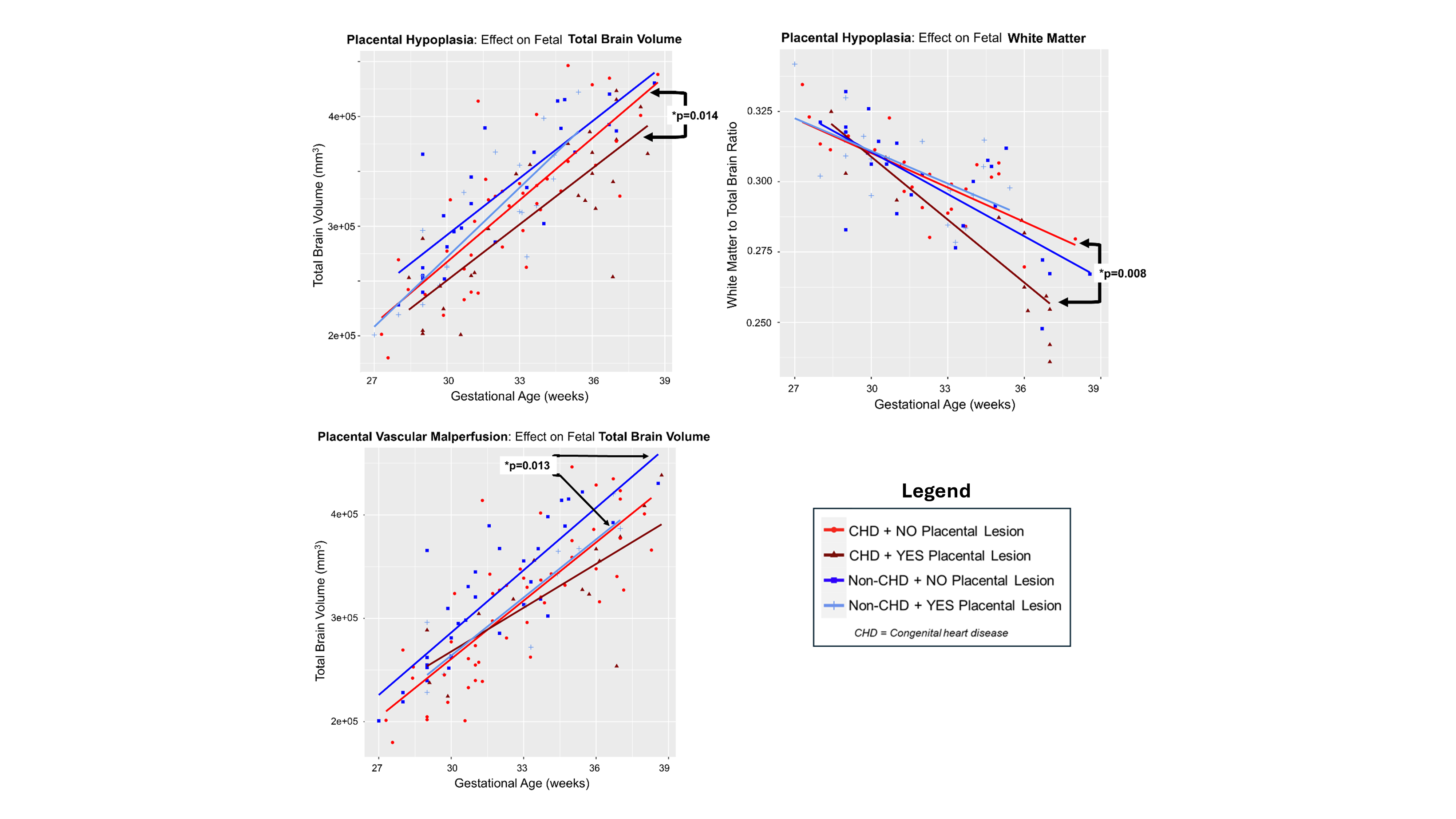 The effect of placental hypoplasia and placental vascular malperfusion on brain volume in fetuses with congenital heart disease (CHD) and those without (non-CHD). A, B) Within the CHD cohort, the presence of placental hypoplasia (defined as placental weight < 10th percentile) is associated with significantly lower total fetal brain volume (p=0.014) and reduced normalized fetal white matter volume (p=0.008). Non-CHD subjects did not show a significant difference between those with and without placental hypoplasia. C) Placental vascular malperfusion (either maternal, fetal, or both) was associated with lower total fetal brain volume in the combined cohort (inclusive of fetuses with and without CHD) (p=0.043), as well as the non-CHD cohort in stratified analysis (p=0.013). Fetuses affected by both CHD and placental vascular malperfusion demonstrated the smallest total brain volumes.
The effect of placental hypoplasia and placental vascular malperfusion on brain volume in fetuses with congenital heart disease (CHD) and those without (non-CHD). A, B) Within the CHD cohort, the presence of placental hypoplasia (defined as placental weight < 10th percentile) is associated with significantly lower total fetal brain volume (p=0.014) and reduced normalized fetal white matter volume (p=0.008). Non-CHD subjects did not show a significant difference between those with and without placental hypoplasia. C) Placental vascular malperfusion (either maternal, fetal, or both) was associated with lower total fetal brain volume in the combined cohort (inclusive of fetuses with and without CHD) (p=0.043), as well as the non-CHD cohort in stratified analysis (p=0.013). Fetuses affected by both CHD and placental vascular malperfusion demonstrated the smallest total brain volumes. 
