Neonatal Clinical Trials 1
Session: Neonatal Clinical Trials 1
552 - Prevalence of Intraventricular Hemorrhage in an RCT of Ventilation During Delayed Cord Clamping: A Subanalysis of the VentFirst Trial
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 552.6408
Marya Strand, Akron Children's Hospital, Brecksville, OH, United States; Dorothy Bulas, Children's National Hospital, Washington dc, DC, United States; Jennifer Fang, Mayo Clinic, Rochester, MN, United States; Karen Fairchild, University of Virginia School of Medicine, Charlottesville, VA, United States; Justin Josephsen, Saint Louis University School of Medicine, Saint Louis, MO, United States; Susan Niermeyer, University of Colorado School of Medicine, Denver, CO, United States; Gina Petroni, University of Virginia School of Medicine, Charlottesville, VA, United States; beth Kline-Fath, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Jamie B. Warren, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States

Marya Strand, MD, MS (she/her/hers)
Chair, Neonatal-Perinatal Medicine
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: Intraventricular hemorrhage (IVH) is a significant morbidity associated with prematurity. The incidence of IVH has changed over time with the evolution of neuroprotective prevention strategies for extremely preterm infants. There is limited data available for the youngest gestational age strata in an era of high maternal antenatal steroid and magnesium administration and delayed cord clamping.
Objective: Describe the distribution of IVH in the extremely preterm population in the VentFirst RCT.
Design/Methods: This is a secondary study of the VentFirst trial, which took place at 12 centers across the US and Canada. This trial randomized the infants of women delivering between 23 0/7 and 28 6/7 weeks gestation to delayed cord clamping for 30 to 60 seconds after birth followed by routine resuscitation (control) or assisted ventilation (CPAP for babies breathing well or positive pressure ventilation for babies not breathing well) from 30 until 120 seconds after birth followed by cord clamping (intervention). Antenatal informed consent was required, and randomization occurred prior to delivery. Each infant had a head ultrasound at 7-10 days after birth which was read by both the local pediatric radiologist at the study site and one of three external pediatric radiologists engaged for the duration of the trial (BKF, ME, DB). All radiologists (local and external) were blinded to study group. Rates of IVH were analyzed by GA strata (23-24 weeks vs 25-28 weeks).
Results: 570 total infants were enrolled in VentFirst. All 549 infants that survived to a first ultrasound (96% of the study population) were included in the analysis. 100% of the mothers received antenatal steroids, and 90% received magnesium on the day of delivery. The population is shown in Table 1.
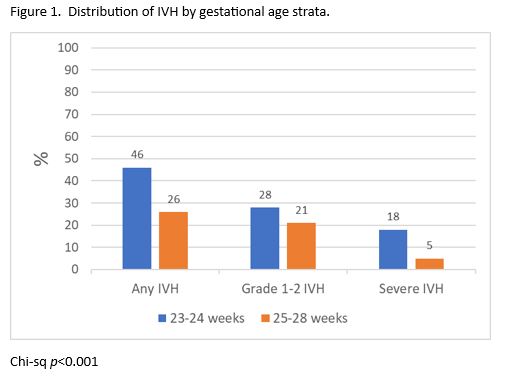
Any IVH and severe (grade 3 or 4) IVH were significantly more prevalent in the lower gestational age strata of this population (Chi sq p< 0.001, Figure 1). The timing of cord clamping, regardless of study group, was not independently associated with presence or grade of IVH. This population of ELBW infants has a lower incidence of IVH compared to historical reports of IVH in a similarly aged population.
Conclusion(s): In this study population with universal exposure to antenatal steroids, preponderance of maternal magnesium and delay in cord clamping, severe IVH was predominantly in the 23-24 week population. This report represents the current incidence of IVH in the extremely preterm population with the advantages of good maternal care.
Table 1. Description of population
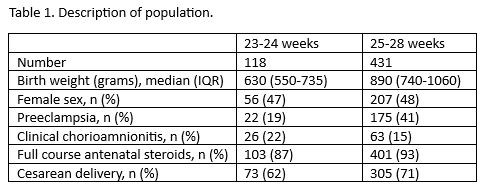
Figure 1. Distribution of IVH by gestational age strata