Nephrology 2
Session: Nephrology 2
018 - Practice Variations in the Management of Edema in Childhood Nephrotic Syndrome: A National Survey
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 18.6287
Siobhan Thornton, University of Saskatchewan College of Medicine, REGINA, SK, Canada; Kayla Flood, Jim Pattison's Children's Hospital, Saskatoon, SK, Canada; Cherry Mammen, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Susan M. Samuel, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada

Siobhan Thornton, MD (she/her/hers)
Resident Physician
University of Saskatchewan College of Medicine
REGINA, Saskatchewan, Canada
Presenting Author(s)
Background: Nephrotic syndrome (NS) is a commonly acquired pediatric kidney disease, often resulting in substantial edema from the accumulation of fluid within the interstitial tissues. Edema management varies widely due to differences in clinical assessment, practice variation, and lack of consensus guidelines. How physicians manage edema within individual clinical scenarios, and the extent of practice variability, remains unclear.
Objective: This study aims to better understand the scope of clinical management of edema for children with NS within Canada, related to: (a) pharmacologic and non-pharmacologic interventions, (b) clinical decision making, and (c) perceived complications.
Design/Methods: We conducted a cross-sectional survey of pediatric nephrologists and trainees across Canada using REDCap®. The survey included a variety of question types (yes/no response, Likert scale, free response), covering demographics, practice variation, and responses to a clinical vignette describing a 3-year-old boy with NS who presented with normal vital signs and laboratory values despite clinical edema and 30% cumulative fluid overload.
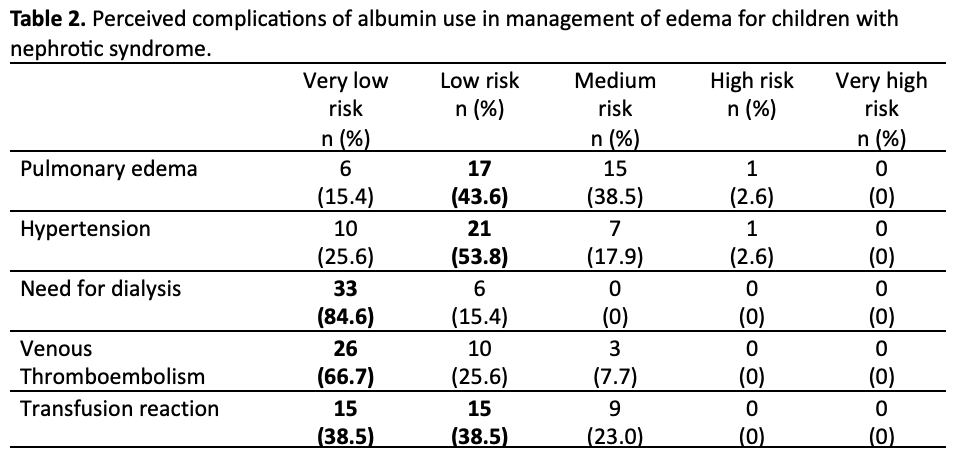
Results: Forty-one pediatric nephrologists and trainees completed the survey, with around half (53.3%) having over 10 years of experience. Respondents felt that patients with a new NS diagnosis required admission primarily due to edema (76.9%) (Table 1). Most (62%) reported an average admission length of 48-72 hours. Admission decisions varied, with 41.2% opting for admission and 38.2% unsure based on the same clinical vignette. A majority (84.6%) frequently used albumin for edema management, perceiving a low risk of complications, though pulmonary edema remained the greatest concern (Table 2). Edema management was primarily stopped based on clinical symptoms (74%), improvements in physical exam findings (63%), and complete resolution of edema (46%). At discharge, 85% of physicians recommended fluid restriction, and all recommended salt restriction during relapses to prevent edema recurrence.
Conclusion(s): Edema remains the primary reason for hospital admission in children with NS, yet there is notable variation in admission criteria and recommended therapies. Albumin infusions are commonly administered, but their application varies widely, and the frequency of related complications remains uncertain. This variability highlights a lack of clinical research and the absence of consensus guidelines for managing edema in NS. Randomized trials studying edema management are essential to establishing evidence-based guidelines and standardized clinical protocols.
Table 1.
.png)
Table 2.