Newborn Care 1
Session: Newborn Care 1
244 - Decreasing Unnecessary Formula Use in Late Preterm and Early Term Breastfed Infants through a Donor Human Milk Voucher Program: A Quality Improvement Project
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 244.4136
Oresta Rule, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Kristin Shadman, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Elizabeth Goetz, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States

Oresta Rule, MD
Assistant Professor
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: At our large Wisconsin-based birthing center, breastfed late preterm and early term infants receive supplemental feedings to limit weight loss while awaiting parental milk production. Parents may choose to supplement with hospital-supplied donor human milk (DHM) or formula. No processes support transition to exclusive breastfeeding for these patients, so those who supplement with formula may continue formula longer than necessary.
Objective: This quality improvement (QI) project aimed to decrease the proportion of breastfed late preterm and early term singleton infants receiving supplemental formula by 30 percentage points (p.p.) at hospital discharge and by 10p.p. at 2-week outpatient visit from November 2023 to September 2024.
Design/Methods: Using QI methodology, a team of newborn hospitalists, outpatient pediatricians, and lactation consultants identified root causes and selected improvement processes to decrease the proportion of late preterm and early term infants receiving supplemental formula. Two changes were implemented using Plan-Do-Study-Act cycles: 1) providing DHM to eligible patients at discharge through a pilot voucher program, and 2) offering standardized discharge feeding instructions with added guidance to stop supplementation. P-charts with 2-week intervals followed process measures, including supplemental formula use at hospital discharge and 2-week visit, and balancing measures, including excessive weight loss and failure to regain birth weight by 2-week visit. Two-week follow-up telephone interviews with parents provided perspectives on supplementation pre and post process changes.
Results: Baseline data (11/1/23-2/29/24) showed the proportion of late preterm and early term infants receiving supplemental formula was 31.5% during birth admission, 58.2% at hospital discharge, and 38.5% at 2-week visit (Figure 1). At baseline, parents cited cost and access of DHM as reasons to transition to formula at discharge and attributed ongoing formula use to ease. After implementing a DHM voucher program (3/1/24-9/17/24), the proportion of infants receiving supplemental formula decreased to 28.2% (-30.0p.p.) at hospital discharge and to 24.8% (-13.7p.p.) at 2-week visit (Figure 1). Balancing measures (Figure 2) were unchanged. Parents reported high satisfaction with the voucher program.
Conclusion(s): We found reducing barriers to DHM access can decrease supplemental formula use at hospital discharge and 2-week visit among late preterm and early term infants. Future work may explore long-term breastfeeding outcomes and feasibility of sustaining and expanding DHM access.
Figure 1. Supplemental Formula Use at Birth Admission, Hospital Discharge, and 2-Week Visit
.jpg) Control charts from 11/1/23-9/17/24 demonstrate a decrease in the biweekly proportion of late preterm and early term singleton infants receiving supplemental formula at hospital discharge and 2-week visit after initiation of a DHM voucher program: supplemental formula use decreased from 58.2% to 28.2% (-30.0p.p.) at hospital discharge and from 38.5% to 24.8% (-13.7p.p.) at 2-week visit. The proportion of infants receiving supplemental formula during birth admission remained unchanged at 31.5%.
Control charts from 11/1/23-9/17/24 demonstrate a decrease in the biweekly proportion of late preterm and early term singleton infants receiving supplemental formula at hospital discharge and 2-week visit after initiation of a DHM voucher program: supplemental formula use decreased from 58.2% to 28.2% (-30.0p.p.) at hospital discharge and from 38.5% to 24.8% (-13.7p.p.) at 2-week visit. The proportion of infants receiving supplemental formula during birth admission remained unchanged at 31.5%.Figure 2. Balancing Measures
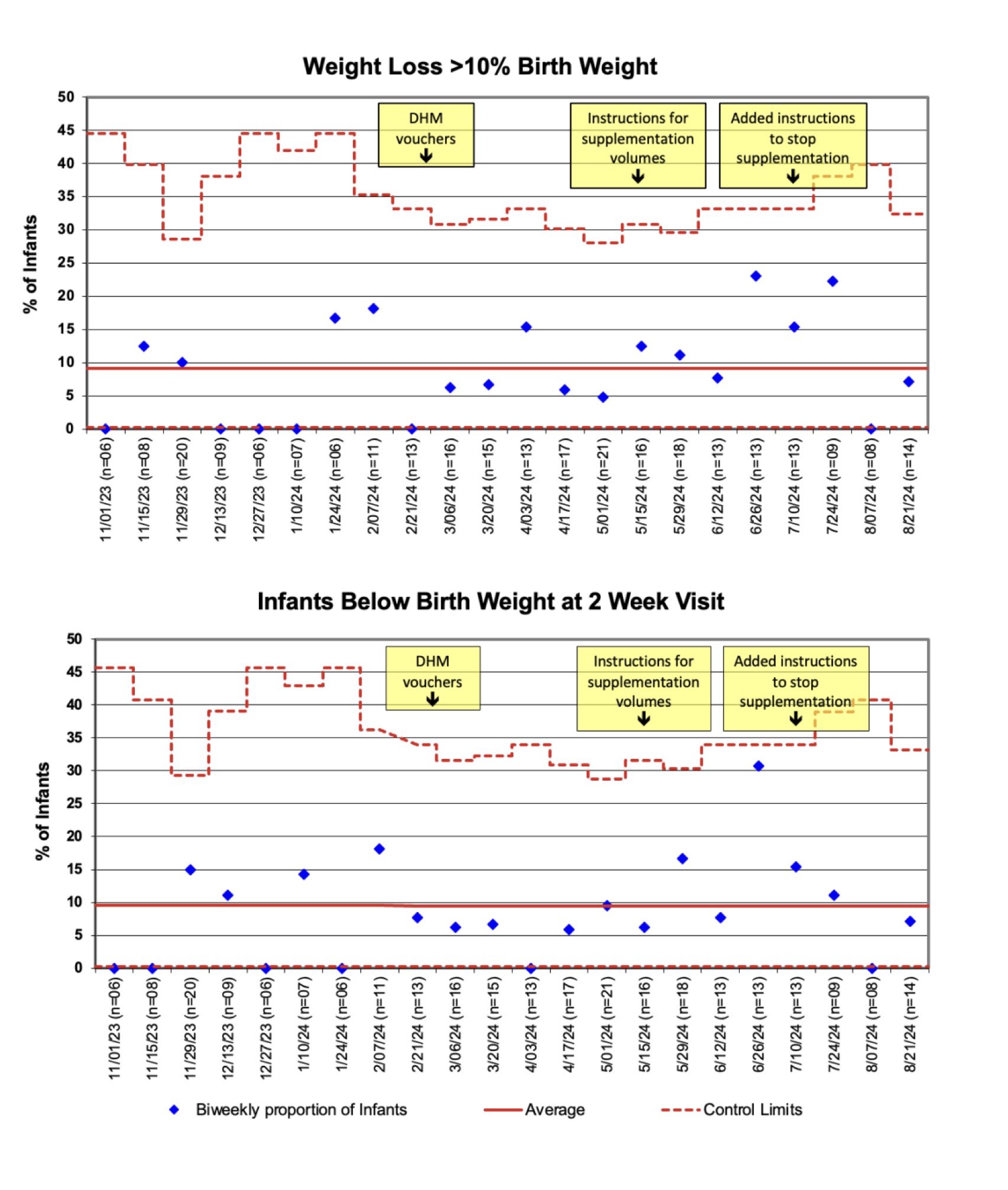 Control charts from 11/1/23-9/17/24 show no change in biweekly proportion of late preterm and early term singleton infants with excessive weight loss (>10% of birth weight) or failure to regain birth weight by 2-week visit.
Control charts from 11/1/23-9/17/24 show no change in biweekly proportion of late preterm and early term singleton infants with excessive weight loss (>10% of birth weight) or failure to regain birth weight by 2-week visit.Figure 1. Supplemental Formula Use at Birth Admission, Hospital Discharge, and 2-Week Visit
.jpg) Control charts from 11/1/23-9/17/24 demonstrate a decrease in the biweekly proportion of late preterm and early term singleton infants receiving supplemental formula at hospital discharge and 2-week visit after initiation of a DHM voucher program: supplemental formula use decreased from 58.2% to 28.2% (-30.0p.p.) at hospital discharge and from 38.5% to 24.8% (-13.7p.p.) at 2-week visit. The proportion of infants receiving supplemental formula during birth admission remained unchanged at 31.5%.
Control charts from 11/1/23-9/17/24 demonstrate a decrease in the biweekly proportion of late preterm and early term singleton infants receiving supplemental formula at hospital discharge and 2-week visit after initiation of a DHM voucher program: supplemental formula use decreased from 58.2% to 28.2% (-30.0p.p.) at hospital discharge and from 38.5% to 24.8% (-13.7p.p.) at 2-week visit. The proportion of infants receiving supplemental formula during birth admission remained unchanged at 31.5%.Figure 2. Balancing Measures
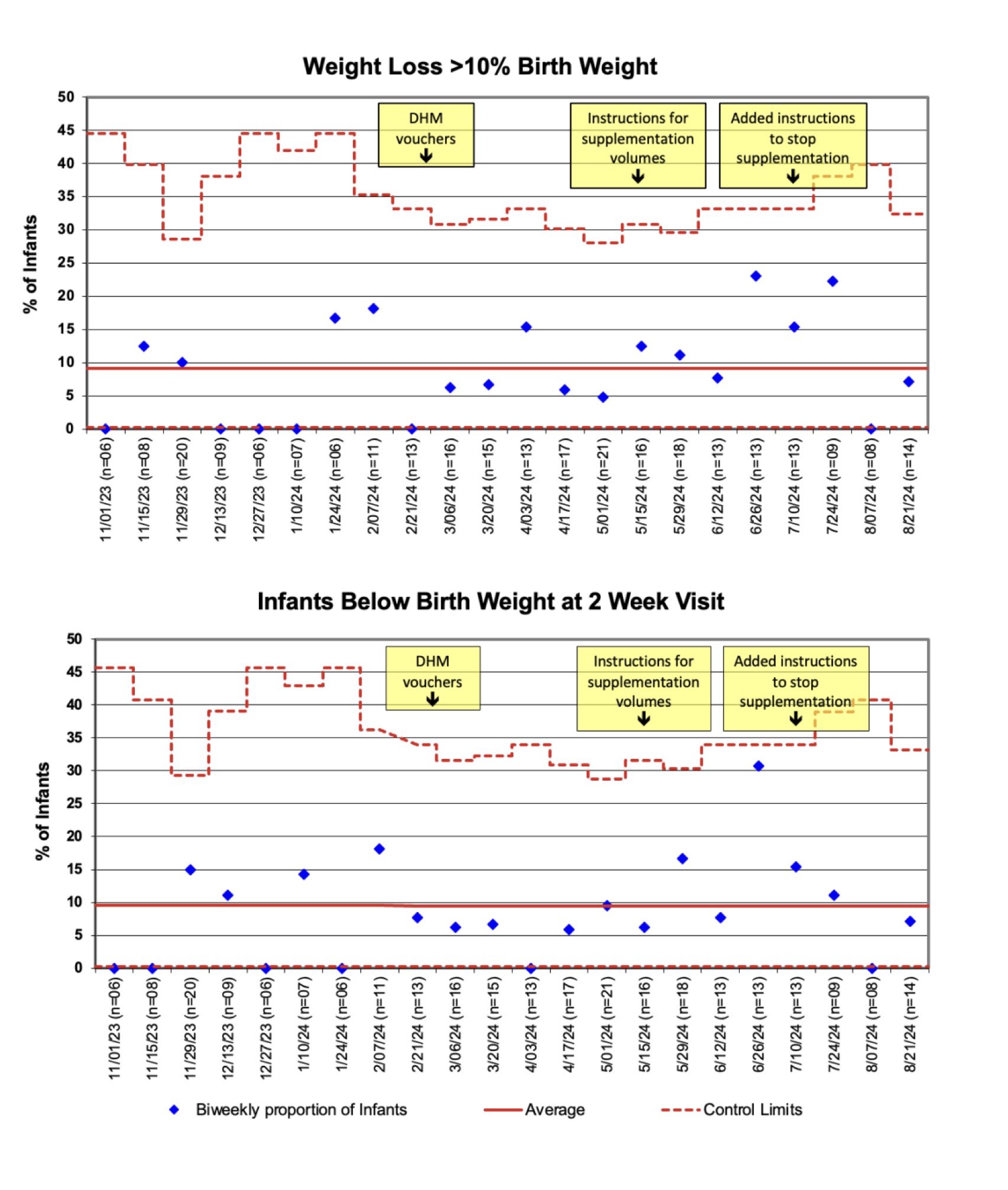 Control charts from 11/1/23-9/17/24 show no change in biweekly proportion of late preterm and early term singleton infants with excessive weight loss (>10% of birth weight) or failure to regain birth weight by 2-week visit.
Control charts from 11/1/23-9/17/24 show no change in biweekly proportion of late preterm and early term singleton infants with excessive weight loss (>10% of birth weight) or failure to regain birth weight by 2-week visit.

