Newborn Care 1
Session: Newborn Care 1
256 - Standardizing Well Infant Hypothermia Clinical Care: Quality Improvement
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 256.6942
Marion M. Bendixen, University of Florida, Winter Park, FL, United States; Elizabeth de Paula Fonseca, UF Health Shands Children's Hospital, Gainesville, FL, United States; Kendall Steadmon, University of Florida College of Medicine, Gainesville, FL, United States
Kendall Steadmon, MD (she/her/hers)
Clinical Associate Professor
University of Florida College of Medicine
Micanopy, Florida, United States
Presenting Author(s)
Background: Despite negative consequences of newborn hypothermia, such as metabolic acidosis, respiratory distress, and infection risk, nationally standardized guidelines for rewarming newborns with mild and moderate hypothermia beyond delivery are lacking. Infant hypothermia (<,36.5°C,) affects 24% of term and 62% of late-preterm newborns within the first 6 hours of life. World Health Organization supports use of skin-to-skin contact, monitoring, and assessments. Mother-baby nurses must rely on their discretion to make infant rewarming decisions. This may manifest in infrequent monitoring, vital signs, and documentation.
Objective: To evaluate prior practices and implement a hypothermia algorithm to address gaps in infant hypothermia care and improve documentation.
Design/Methods: This QI project (QIPR ID: 2249) followed a Plan Do Study Act (PDSA) model. Retrospective electronic health record (EHR) audit included all newborns who became hypothermic on the mother-baby unit over 5-weeks followed by 4 PDSA 5-week cycles. Multidisciplinary team developed hypothermia treatment algorithm to standardize identification, interventions, and provider notification (figure 1). Smart Phrase, (EHR common text insert) was created to standardize documentation and prompt interventions (figure 2). Descriptive and t-test comparison analysis of pre-post algorithm implementation of vital sign assessments, blood glucose measurements, and provider notification. Effectiveness of the treatment approaches evaluated with GLMM analysis based on the time taken to achieve normothermia (≥36.5°C).
Results: Pre-implementation 5-week EHR audit (n=20) through 4 PDSA cycles (20 weeks, n=64) revealed use of skin-to-skin contact for rewarming increased from 30% to 73%. Within 1-hour of infant hypothermia, provider notification increased 20% to 67% (p=0.0003) and blood glucose assessments 55% to 92% (p=0.0003). Hypothermia to normothermia average time decreased from 72 to 48 minutes. Examining factors including birth weight, maternal temperature, 5-minute APGAR score, delivery type, analgesia type, initial low temperature, and infant age (hours) found infant age (0.0455) influenced skin-to-skin rewarming failure.
Conclusion(s): Pre-project EHR review exposed variances in rewarming practices. Standardized algorithm implementation has led to measurable improvements in infant hypothermia care including increased documentation compliance, provider notification and skin-to-skin utilization, thus decreasing mother/infant separation. Continued monitoring of our practices incorporating documentation tools and smart phrases may further enhance evidence-based care.
Figure 1. Example Smart Phrase
Figure_1_PAS_abstract_Bendixen.pdfSmart phrase used to document infant hypothermia event. Bold font areas indicate fields to be filled in by the nurse.
Figure 2. Newborn Hypothermia Treatment Algorithm
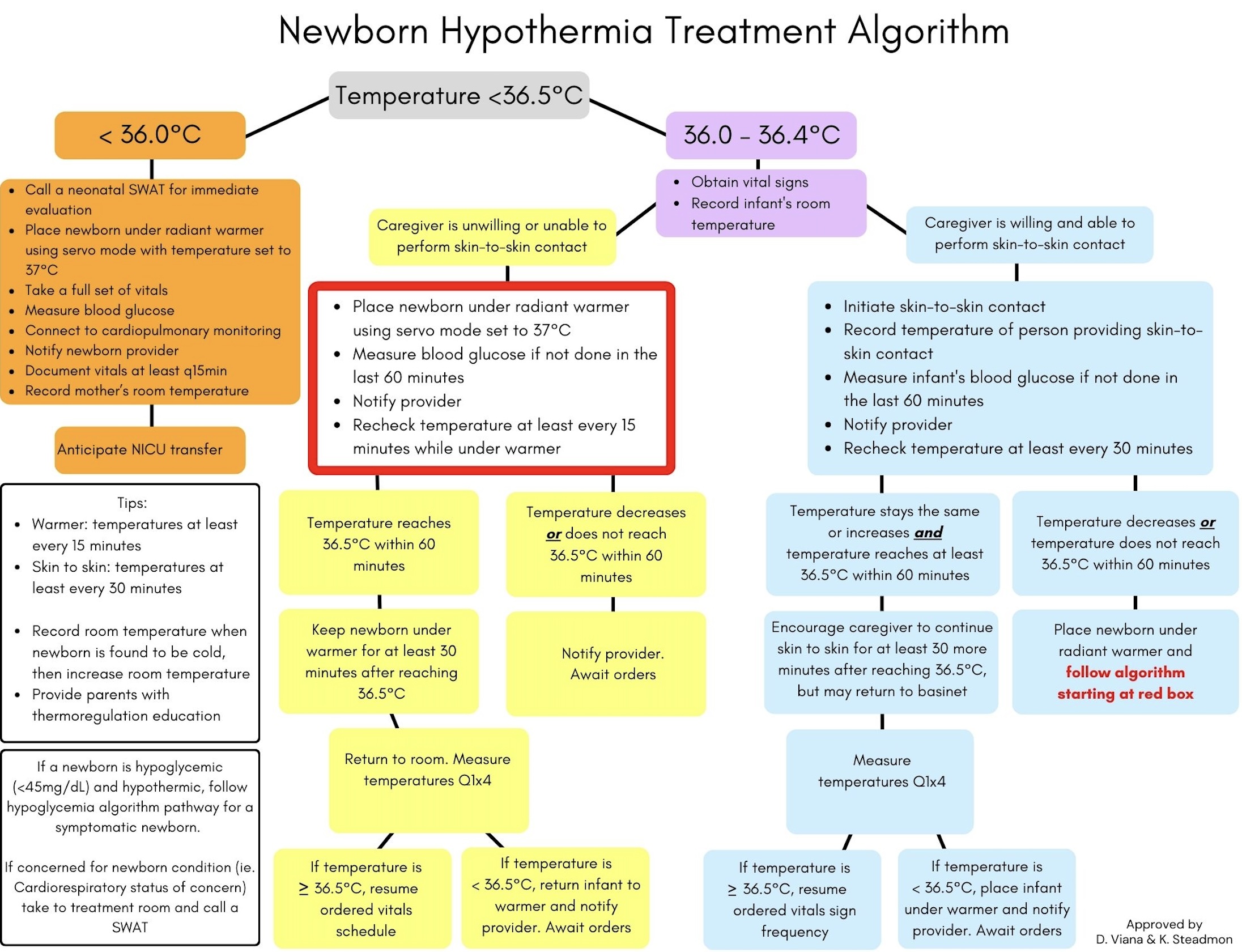 Example of the newborn hypothermia treatment algorithm implemented in the QI project.
Example of the newborn hypothermia treatment algorithm implemented in the QI project.
