Neonatal Neurology 4
Session: Neonatal Neurology 4
660 - Identifying Priorities in Long-term Follow-up Care for Children with Hypoxic-Ischemic Encephalopathy: Insights from a Parent and Provider Survey
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 660.5464
Andrea C.. Pardo, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Niranjana Natarajan, University of Washington School of Medicine, Seattle, WA, United States; Danielle Guez-Barber, Children's Hospital Colorado, Aurora, CO, United States; Betsy Pilon, Hope for HIE, West Bloomfield, MI, United States; Alexa K. Craig, The Barbara Bush Children's Hospital at Maine Medical Center, Scarborough, ME, United States

Andrea C. Pardo, MD, FAAP, FCNS (she/her/hers)
Associate Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Neonatal hypoxic-ischemic encephalopathy (HIE) significantly impacts child development, increasing risks for cognitive, motor, and behavioral disabilities. HIE is also associated with an increased risk of epilepsy and infantile spasms (IS). At present, there are no evidence-based guidelines for the long-term follow-up of children after HIE, including recommendations for IS screening.
Objective: To identify gaps in care and understand stakeholder perspectives from both parents and providers to inform the development of comprehensive follow-up guidelines.
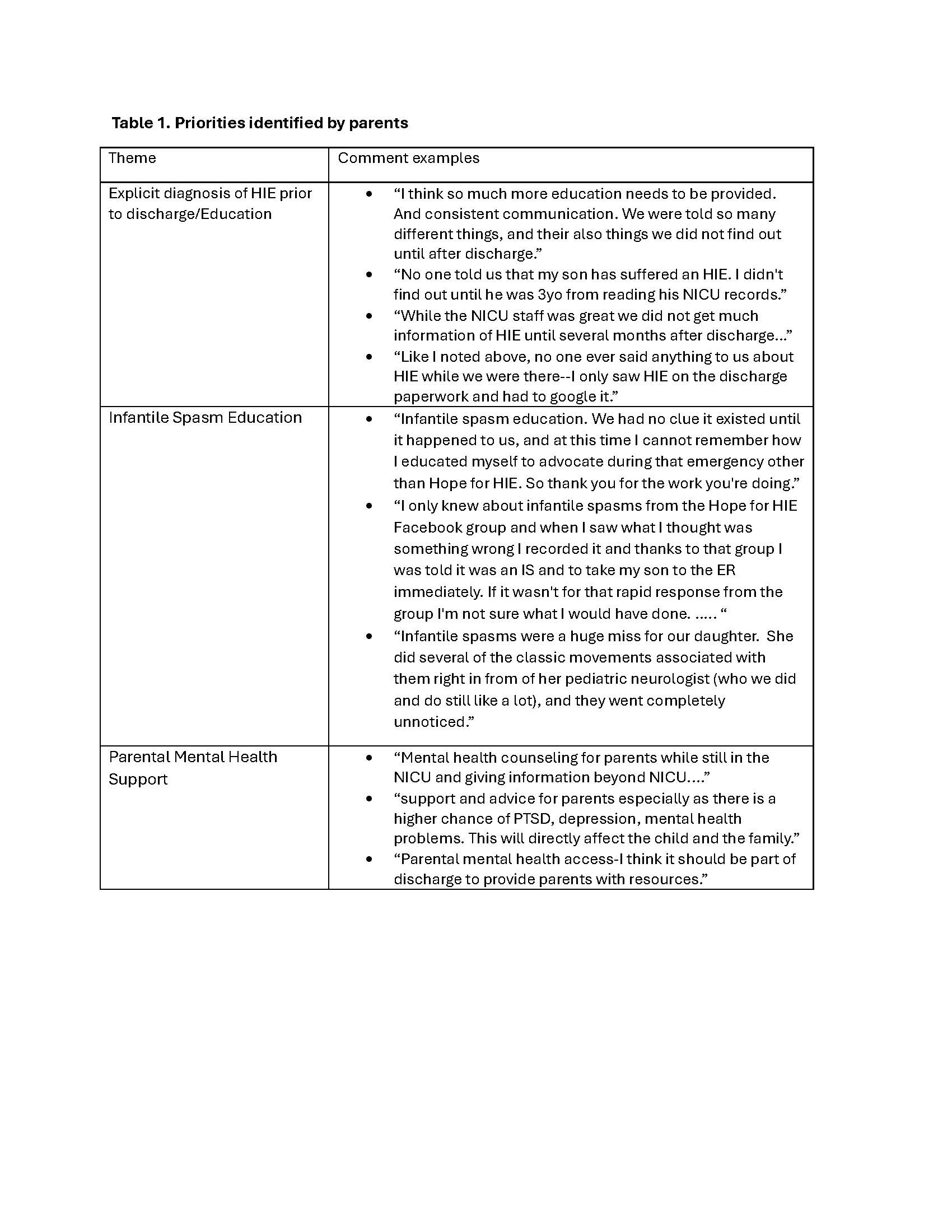
Design/Methods: Two separate self-administered surveys, open from 10/11/24 to 10/25/24, were distributed to parents via Hope for HIE and providers via the Child Neurology Society website, Newborn Brain Society listserv, and social media sites. The surveys were created by a work group consisting of child neurologists and parents of children with HIE. Data were analyzed using descriptive statistics. Open ended comments were reviewed for themes (Table 1).
Results: Two hundred fifty-eight parental responses were analyzed, primarily from high-income countries (71%), with most children born in the past five years (50%). Respondents predominantly had children with moderate to severe HIE (75%); 25% reported no impairment, 25% mild (e.g., ADHD, sensory impairments), 25% moderate (e.g., Cerebral Palsy GMFCS I-III, Epilepsy, cognitive impairments), and 24% severe (e.g., Ventilator, G-Tube, Cerebral Palsy GMFCS IV/V). Regarding IS, 82% of parents reported receiving no specific counseling about IS. 54% of parents report having a repeat EEG performed after discharge.
Among the 88 providers who responded (majority child, neonatal and/or fetal neurologists), the primary factors guiding HIE follow-up were severity of encephalopathy, abnormal MRI, and EEG background. Counseling practices for IS varied: 8% of providers never counseled, 10% counseled if MRI was abnormal, 13% after neonatal seizures, 28% based on clinical concerns, and 20% counseled all parents. Regarding practices for obtaining outpatient EEG, 2% get EEG in all patients with HIE, 13% in patients with seizures during admission and 69% only if there are clinical concerns. There was no consistency in the free text responses regarding timing of EEG, but all responses suggested the first months of life.
Conclusion(s): The surveys revealed a lack of IS counseling for many parents and significant variability among providers, often based on clinical indicators. Further collaboration between families and providers is essential to standardize IS counseling as a core component of long-term follow-up for children with HIE.
Priorities identified by parents