Nephrology 2
Session: Nephrology 2
028 - Assessing the Impact of Prematurity and Neonatal History on Adolescent and Adult Renal Function
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 28.3888
Tyler Shimfessel, University of Texas Southwestern Medical School, Dallas, TX, United States; Gregory Barton, UT Southwestern Medical Center, Dallas, TX, United States; Kara N. Goss, University of Texas Southwestern Medical School, Dallas, TX, United States

Tyler Shimfessel, MD
Resident
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Chronic Kidney Disease (CKD) is a major health epidemic, affecting approximately 35.5 million people in the US and costing patients over $13,000 annually. Preterm birth (≤37 weeks' gestation) affects roughly 1 in 10 births and is associated with a nearly twofold increase in risk of CKD. However, long-term data on renal function in US-born preterm population is lacking.
Objective: Assess kidney function in a cohort of adolescents and adults born preterm between 1986 and 2006, and secondarily to assess how risk factors, such as degree of prematurity and neonatal history, impact later life renal function.
Design/Methods: Using the Parkland Hospital NICU Registry, patients aged 12-40 years born ≤32 weeks gestation or < 1500 g were recruited for a prospective study, along with healthy term-born similarly aged participants from Dallas County. Study procedures included anthropometrics, vitals, pulmonary function, echocardiography, sleep assessment, and basic laboratory testing. Here, we present renal function parameters. Data are reported as mean (SD). To assess how neonatal factors may impact risk of subsequent renal dysfunction, we considered bronchopulmonary dysplasia (BPD), sepsis, and symptomatic patent ductus arteriosus (PDA) as potential nephrotoxic risk states for which data was available in the Parkland NICU Registry. Multivariate linear regression was used to determine the main effect of neonatal and adult factors separately on markers of renal function.
Results: Participants included 103 preterm and 43 term individuals. Patients born prematurely had significantly lower Creatinine and higher Glomerular Filtration Rate (GFR). Cystatin C trended higher after preterm birth. Multivariate linear regression demonstrated that gestational age and Cystatin C were significantly related to GFR, where lower GA associated with higher GFR and higher cystatin C associated with lower GFR (p= 0.0008, R2= 0.096). The presence or accumulation of potential nephrotoxic risk states in the neonatal period did not correlate with subsequent renal function.
Conclusion(s): Those born prematurely had lower Creatinine and higher GFR overall, with a strong association between GFR and gestation age, suggesting a potential hyperfiltrative state following preterm birth. Adjustment for Cystatin C may identify subclinical renal dysfunction in the preterm population, warranting evaluation with further functional testing.
Table 1
.png)
Figure 1
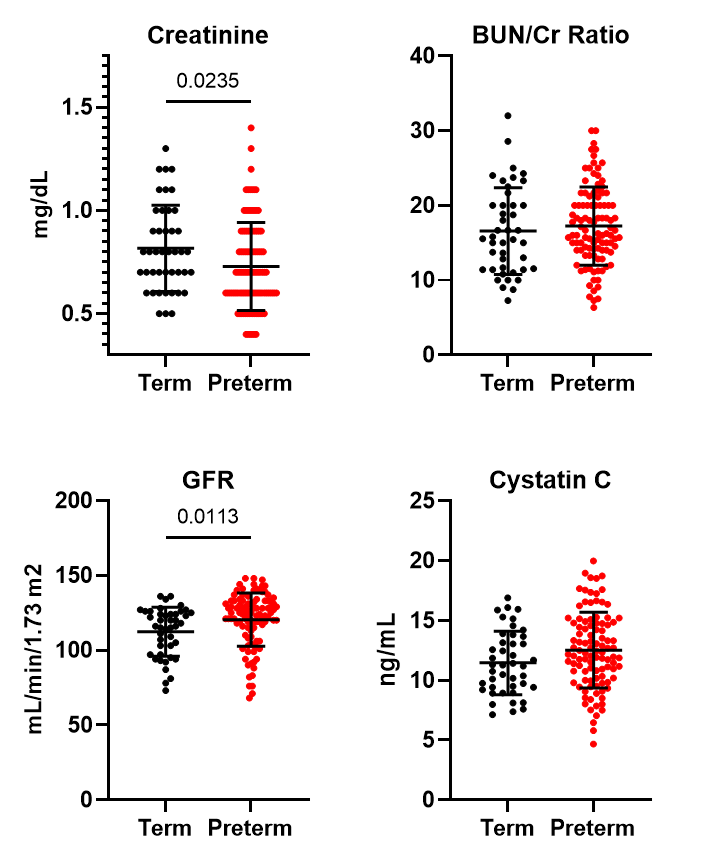 Adolescents and adults born prematurely exhibit reduced Creatinine (p=0.024) and higher Glomerular Filtration Rate (GFR) (p=0.011) compared to term-born participants.
Adolescents and adults born prematurely exhibit reduced Creatinine (p=0.024) and higher Glomerular Filtration Rate (GFR) (p=0.011) compared to term-born participants.
