Nephrology 2
Session: Nephrology 2
016 - LDL apheresis in pediatric patients with multi-drug resistant idiopathic nephrotic syndrome or recurrent FSGS in a kidney transplant.
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 16.5577
Julia W. McDonald, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Juhi Kumar, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Armando J. Ganoza, UPMC Childrens Hospital of Pittsburgh, PITTSBURGH, PA, United States; Michael L. Moritz, UPMC Children's, Pittsburgh, PA, United States

Julia W. McDonald, MD (she/her/hers)
Pediatric Nephrology Fellow
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Idiopathic nephrotic syndrome is steroid resistant in approximately 15% of pediatric patients, of which 30-50% will be calcineurin inhibitor resistant requiring multidrug therapy (Trautman, 2020). The primary cause of multi-drug resistant nephrotic syndrome (MRNS) is focal segmental glomerulosclerosis (FSGS), which has a high risk of progression to end stage kidney disease (ESKD). FSGS is the most prevalent cause of acquired ESKD in children and recurs in approximately 50% of kidney transplants (Shah, 2019). LDL apheresis (LDL-A) was approved by the FDA in 2013 as a Humanitarian Use Device (HUD) in pediatric patients for the treatment of FSGS that is resistant to therapy or that recurs in the kidney transplant (rFSGS) as the effectiveness of LDL-A is uncertain.
Objective: To evaluate the effectiveness of LDL-A in achieving short and long-term remission in pediatric patients with MRNS or rFSGS.
Design/Methods: We conducted a retrospective chart review of six pediatric patients at UPMC Children’s Hospital of Pittsburgh treated with various durations of LDL-A in conjunction with steroids for MRNS or rFSGS. The duration of therapy was individualized based on the patient’s response to therapy. Data collection included disease onset, biopsy results, immunosuppressive therapy, indications for initiating LDL-A, duration of LDL therapy, and short- and long-term outcomes on proteinuria, hypoalbuminemia, and kidney function.
Results: Following IRB approval, six pediatric patients, ages 6–18 years, were treated with between 9 and 30 weeks of LDL-A with 2.5 to 8 years of follow up. Five of the six patients (Cases 1 -5) achieved complete long-term remission. Two patients with MRNS achieved long-term remission (Table 1, Cases 1-2). Case 2 had late relapses that were responsive to steroids and B-cell depletion. Three of four patients with rFSGS achieved a long-term remission with Case 6 progressing to ESKD within one year of transplant (Table 2, Cases 3-6). Case 4 had late relapses that were responsive to steroids and B-cell depletion. The patients who responded to therapy all had preserved kidney function.
Conclusion(s): LDL-A was effective in achieving a long-term remission of nephrotic syndrome in (83%) of pediatric patients with MRNS or recurrent FSGS in the kidney transplant. Patients who relapsed were responsive to immunosuppressive therapy.
Table 1. Multidrug Resistant Nephrotic Syndrome
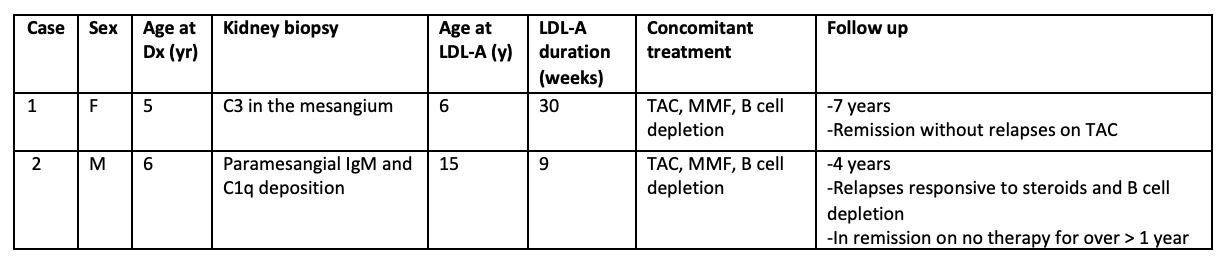 Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)
Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)Table 2. Recurrent FSGS following Kidney Transplant
.jpg) Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)
Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)Table 1. Multidrug Resistant Nephrotic Syndrome
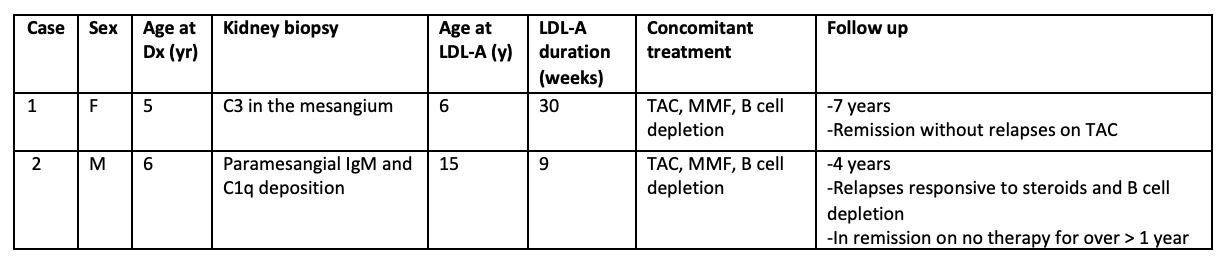 Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)
Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)Table 2. Recurrent FSGS following Kidney Transplant
.jpg) Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)
Therapeutic plasma exchange (TPE), Tacrolimus (TAC), Mycophenolic acid (MMF)
