Emergency Medicine 8
Session: Emergency Medicine 8
116 - Neuroimaging in Children Presenting by Ambulance for Acute Neurological Symptoms
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 116.5593
Rachel Pearson, CHOC Children's Hospital of Orange County, Orange, CA, United States; Nancy Hills, UCSF Benioff Children's Hospital San Francisco, Mill Valley, CA, United States; Kellie Bacon, CHOC Children's Hospital of Orange County, Orange, CA, United States; Shelby K. Shelton, Children's Hospital of Orange County, Orange, CA, United States; Rowena A. Roque, CHOC Children's Hospital of Orange County, Corona, CA, United States; Tatiana R. Moreno, CHOC Children's Hospital of Orange County, Huntington Beach, CA, United States; Maria Kuchherzki, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Carl Schultz, University of California, Davis, School of Medicine, Santa Ana, CA, United States; Theodore Heyming, CHOC Children's Hospital of Orange County, Orange, CA, United States; Heather Fullerton, University of California San Francisco, San Francisco, CA, United States

Rachel Pearson, MD (she/her/hers)
Pediatric Neurologist
CHOC Children's Hospital of Orange County
Orange, California, United States
Presenting Author(s)
Background: In recent years, many pediatric hospitals have developed “brain attack” pathways to facilitate emergent imaging for children presenting with acute neurological symptoms, particularly those concerning for stroke. Rapid diagnostic imaging is essential given the time-sensitivity of acute stroke interventions. MRI is the preferred imaging modality for acute ischemic stroke (AIS). While pediatric stroke is rare, children presenting with acute neurological symptoms from other causes can also benefit from expedited imaging to determine a diagnosis and guide interventions.
Objective: Describe the current state and inform quality improvement efforts aimed at optimizing the time from emergency medical services (EMS) activation to neuroimaging for children with acute neurological symptoms.
Design/Methods: This is a retrospective study of 1–14-year-olds with an EMS activation for acute neurological symptoms (based on EMS primary symptom and impression codes) who were transported to a pediatric emergency department between 1/2019-6/2023. We excluded patients with a diagnosis of epilepsy or major trauma and inter-facility transfers. We used descriptive statistics to explore neuroimaging frequency and modality, time to imaging, and frequency of actionable findings.
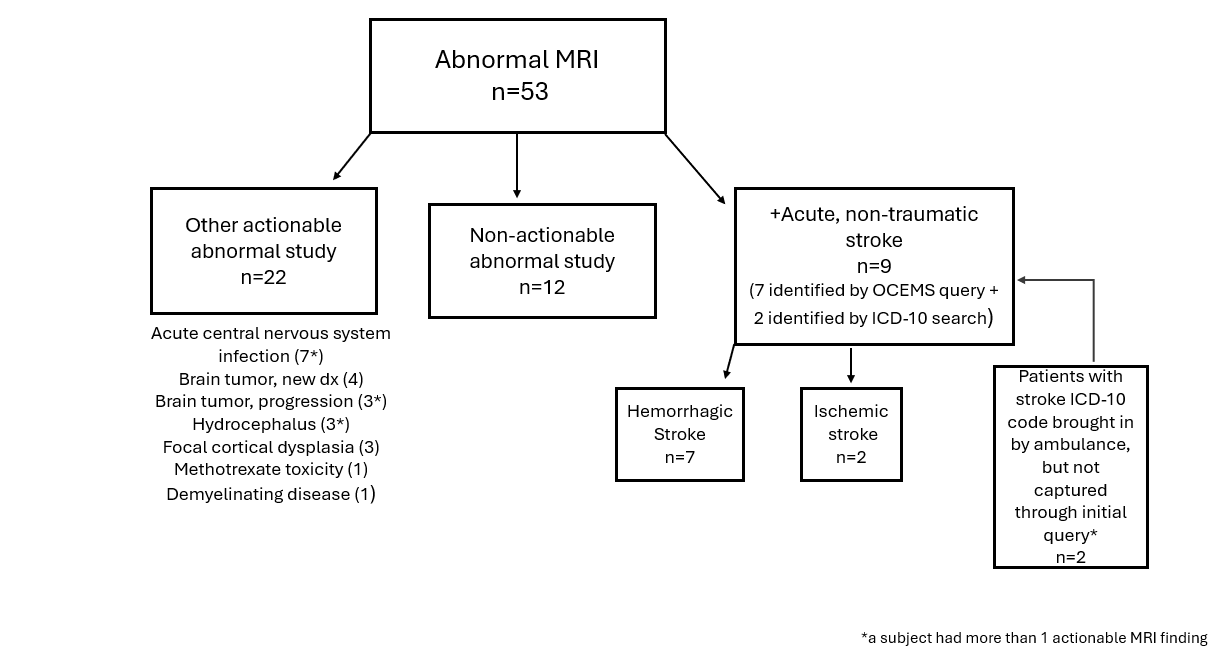
Results: Of 3888 children with EMS activations for acute neurological symptoms, 695 (17.9%) had neuroimaging. 570 (82.0%) had CT scan only; 125 (18.0%) also had MRI. Of the patients that had MRI, 31 (24.8%) had actionable abnormal studies. The most common actionable finding was stroke, followed by central nervous system infection and newly diagnosed brain tumor (Figure 1). The median (IQR) times to imaging were 2.29 (1.56, 3.21) and 26.8 (16.3, 48.8) hours to CT and MRI, respectively. Hispanic children were less likely to have any neuroimaging compared to patients of other races/ethnicities (p < 0.001), regardless of primary spoken language.
Conclusion(s): Among children with EMS activations for acute neurological symptoms selected for neuroimaging, CT was the imaging modality of choice, despite its low sensitivity for AIS (established in radiology literature). Subsequent MRI is often delayed >24 hours, beyond the current window for acute stroke therapies. The lower imaging rates in Hispanic children suggest possible bias or a gap in cultural competency that should be further explored. These findings suggest opportunities to improve care pathways for children presenting with acute neurological symptoms and will inform a future study in which we plan to reassess times to imaging after an educational intervention.
Figure 1. Findings in Children with Acute Neurological Symptoms and Abnormal MRI
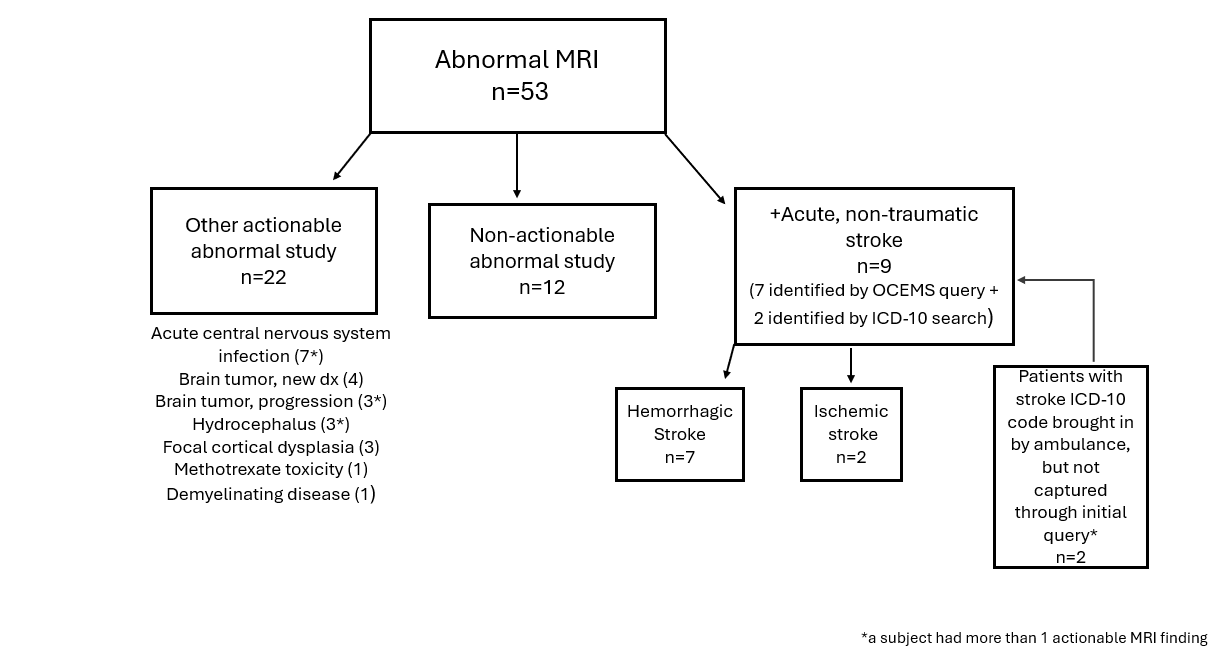
Figure 1. Findings in Children with Acute Neurological Symptoms and Abnormal MRI