Hospital Medicine 4: Medical Education
Session: Hospital Medicine 4: Medical Education
158 - Implementation of Pediatric post-Hospital Outreach Needs Evaluation (PHONE)
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 158.5552
Amanda Klafter, The Children's Hospital at Montefiore, New York, NY, United States; Brenda Anosike, Albert Einstein College of Medicine, Bronx, NY, United States

Amanda Klafter (she/her/hers)
Senior Study Coordinator
The Children's Hospital at Montefiore
New York, New York, United States
Presenting Author(s)
Background: Parents frequently have questions after their child's hospital discharge, covering clinical issues like new symptoms and medication reactions, as well as logistical concerns such as follow-up appointments. While the existing literature emphasizes the importance of post-discharge communication, gaps remain in understanding specific call trends.
Objective: This study investigates these trends at a large-sized, academic children’s hospital located in the Bronx, NY to identify opportunities for enhancing patient education and improving discharge processes.
Design/Methods: We conducted a single-center, cross-sectional observational study to analyze phone calls made by caregivers of pediatric patients recently discharged over an 8-month period from February to October 2024. Inclusion criteria included calls made by legal caregivers of patients aged 0 to 21 years, while calls from healthcare professionals or misdials were excluded. After reaching the target sample size, calls were systematically categorized using a grounded theory approach. Inductive reasoning and coding facilitated thematic analysis. Calls were classified as clinical if they fell within a physician's scope of response, leading to three identified domains: return of symptoms (ROS), new medical problem (NMP), and medication (MED). Non-clinical calls were further categorized as system (S), provider (P), or individual (I).
Results: A total of 32 calls were collected, with an average time of 3 days post-discharge. Questions were evenly split between clinical and non-clinical categories, predominantly occurring at the beginning and end of the week, especially in July. The most common clinical questions concerned medication dosing (50%), while non-clinical inquiries primarily focused on system-level issues (63%). Notable discrepancies were found between the discharged population and the caregivers who called back, particularly regarding Hispanic ethnicity (55% vs. 27%), preferred language (English: 68% vs. 84%), and Medicaid insurance coverage (80% vs. 72%).
Conclusion(s): Our findings underscore the need for enhanced post-discharge communication, as caregivers frequently seek clarity on clinical and logistical issues. The trends in call types and timing can guide targeted patient education strategies, boosting caregiver confidence and reducing anxiety. Furthermore, the demographic discrepancies indicate a need for tailored support for diverse caregiver populations. Understanding these call patterns will enable healthcare providers to refine discharge processes and improve patient outcomes.
Figure 1
.png) The proportion of non clinical calls to clinical calls per day of the week.
The proportion of non clinical calls to clinical calls per day of the week.Figure 2
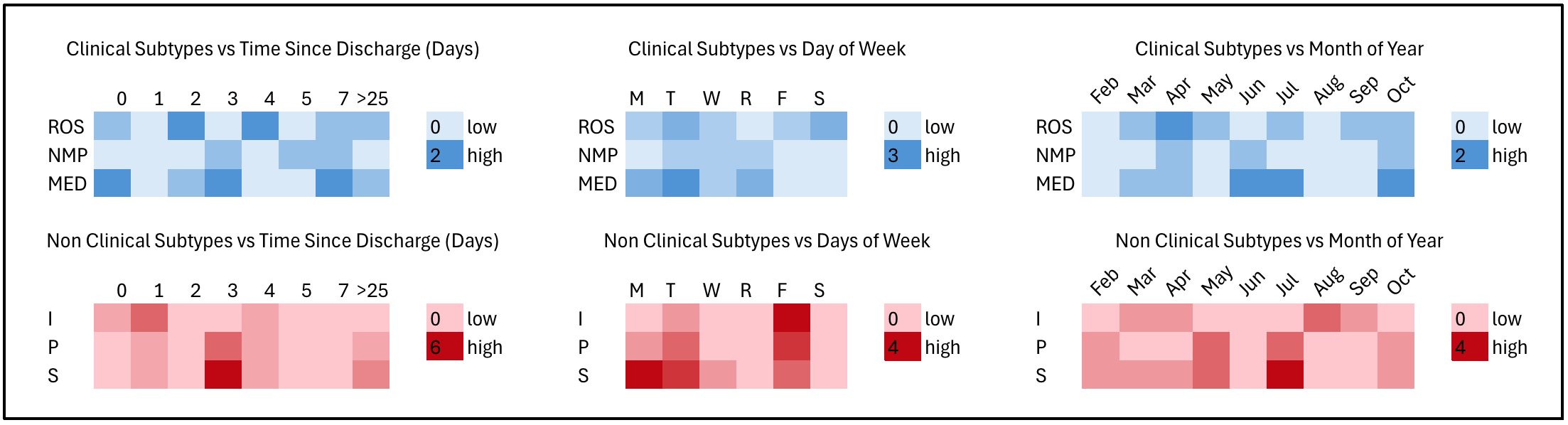 Heat maps show the relative density of call sub-categorization over time, with the lightest color indicating zero occurrences and the darkest representing the highest.
Heat maps show the relative density of call sub-categorization over time, with the lightest color indicating zero occurrences and the darkest representing the highest.
