Hospital Medicine 4: Medical Education
Session: Hospital Medicine 4: Medical Education
160 - Navigating the shifting sands of teaching and faculty-only teams in a pediatric hospital
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 160.5847
Monisha Sachdev, University of Michigan Medical School, Ann Arbor, MI, United States; Jodi Ehrmann, University of Michigan Medical School, Ann Arbor, MI, United States; Maria S. Skoczylas, University of Michigan Medical School, Ann Arbor, MI, United States; Zarina S. Norton, University of Michigan Medical School, Ann Arbor, MI, United States; Harlan McCaffery, University of Michigan Medical School, Ann Arbor, MI, United States; Rebekah Shaw, University of Michigan Medical School, Ann Arbor, MI, United States; Emily Jacobson, University of Michigan Medical School, Ann Arbor, MI, United States

Monisha Sachdev, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Historically, academic hospitalists attend on resident teaching teams. Due to increasing pediatric hospital volumes, emphasis on trainee workload and changing ACGME requirements, the classic hospitalist role is changing. As many look to institute faculty-only hospital medicine teams, little exists in the literature on how team structures impact patient outcomes and hospital throughput within pediatric hospital medicine (PHM).
Objective: To examine the impact of creation of a faculty-only team on patient flow and safety at an academic children’s hospital.
Design/Methods: In November 2022, PHM resident team patient cap was reduced, and a faculty-only hospital medicine team was created for low acuity and expected short length of stay (LOS) patients when resident teams reached cap. PHM patient data were collected pre- (10/2021-10/2022) and post-intervention (12/2022-12/2023). Outcomes included hospital LOS, rapid response team (RRT) initiation, transfer to intensive care unit (ICU), priority discharge (PD) (discharge before 11am), and readmission within 30 days of discharge. We compared outcomes pre- and post-intervention, and based on team structure. Statistical analysis was performed via run chart along with z-test of proportions for categorical variables and t-test for continuous variables.
Results: Average monthly PHM discharges (289 vs 320, p = 0.11) and daily 8 am resident team censuses (13.3 vs 13.3, p = 0.94) were similar pre- and post-intervention. RRT initiation rate (RRTs per total discharges) was lower for PHM patients post-intervention (8.3% vs 7.0%, p = 0.026) with fewer RRTs initiated on the faculty-only team than resident team (4.9 vs 7.2%, p = 0.002). Transfer to ICU per 100 RRTs did not differ pre- vs post-intervention (48.1 vs 56.5, p = 0.057) (Figure 1). Despite similar LOS between resident and faculty-only teams (5.6 vs 4.6 days, p = 0.188) (Figure 2), a higher percentage per month of patients on the faculty-only team had PDs (11.7% vs 8.4%, p = 0.019) without an increase in readmissions (8.1% vs 7.2%, p = 0.56). There was no difference in PDs for all PHM patients pre- vs post-intervention (7.4% vs 8.6%, p = 0.12).
Conclusion(s): Amidst increasing pediatric hospital census, we demonstrated several benefits with the institution of a faculty-only team. A lower rate of RRT initiations suggesting improved ability to think critically with the multidisciplinary team. Increase in PDs on a faculty-only team improves hospital throughput. By demonstrating a benefit to patient safety and flow, this study could lay the groundwork for other institutions as hospital teams are restructured.
Figure 1: ICU transfer per 100 RRTs across teams
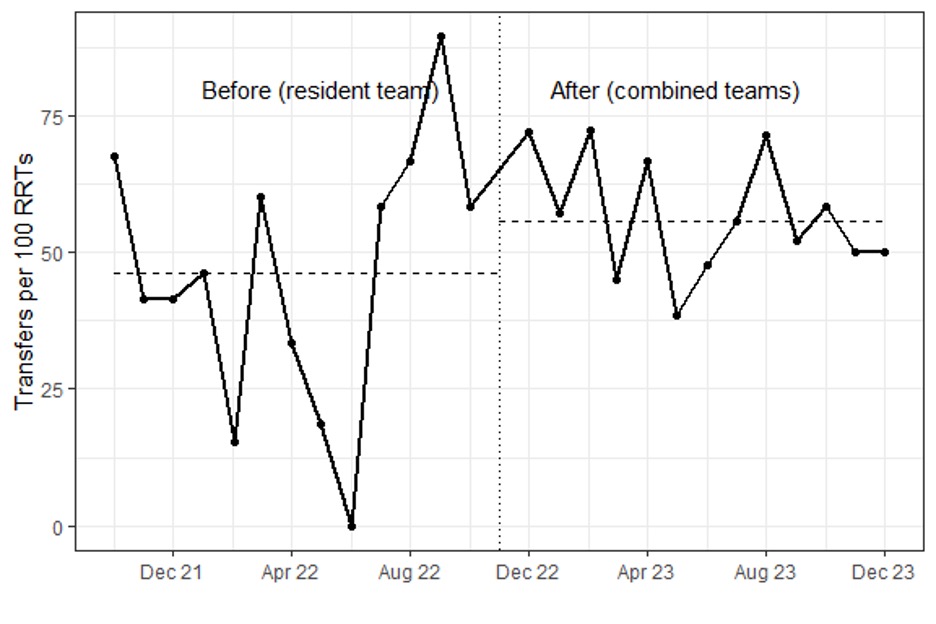
Figure 2: Mean length of stay for resident and faculty-only teams
.jpg)

