Health Equity/Social Determinants of Health 4
Session: Health Equity/Social Determinants of Health 4
700 - Meeting Families Where They Are: Co-Designing for Breastfeeding Success for Rural Mother-Baby Dyads Impacted by Opioid Use Disorder
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 700.6015
Kathryn Dee L. MacMillan, Children's Hospital at Dartmouth-Hitchcock, Lebanon, NH, United States; Karen L. Fortuna, Geisel School of Medicine at Dartmouth, Pembroke, NH, United States; Olivia Siroonian, Geisel School of Medicine at Dartmouth, Duxbury, MA, United States; Meagan Adams, Dartmouth Health, West Lebanon, NH, United States; Haley S. Martell, dartmouth health, lebanon, NH, United States
- KM
Kathryn Dee L. MacMillan, MD MPH
Newborn Nursery Medical Director
Children's Hospital at Dartmouth-Hitchcock
Lebanon, New Hampshire, United States
Presenting Author(s)
Background: Rural obstetric and pediatric patients are disproportionately affected by opioid use disorder (OUD) and sequelae of prenatal opioid exposure. They are less likely to initiate or sustain breastfeeding (BF), hindered by hospital-centric policies, maternal trauma histories, perceived stigma, and inadequate access to social/medical support. Community-based participatory research programs (CBPRP) engage non-researcher stakeholders to design studies with improved relevance, acceptance, and effectiveness.
Objective: This Partnership Academy, a CBPR model, was developed to co-design a remote BF intervention for opioid exposed newborns (OEN) and their families receiving care in rural areas.
Design/Methods: Participants engaged in team-based structured activities designed to build partnerships and engagement. This fosters interactive discussions and problem-solving exercises facilitating shared decision-making, mutual understanding, and actionable strategies for addressing complex health challenges. Participants included lived experience experts, recovery support workers, doulas, certified lactation counselors, social workers and pediatricians. Qualitative analysis of transcripts was performed using the Rigorous and Accelerated Data Reduction (RADaR) technique and member checking.
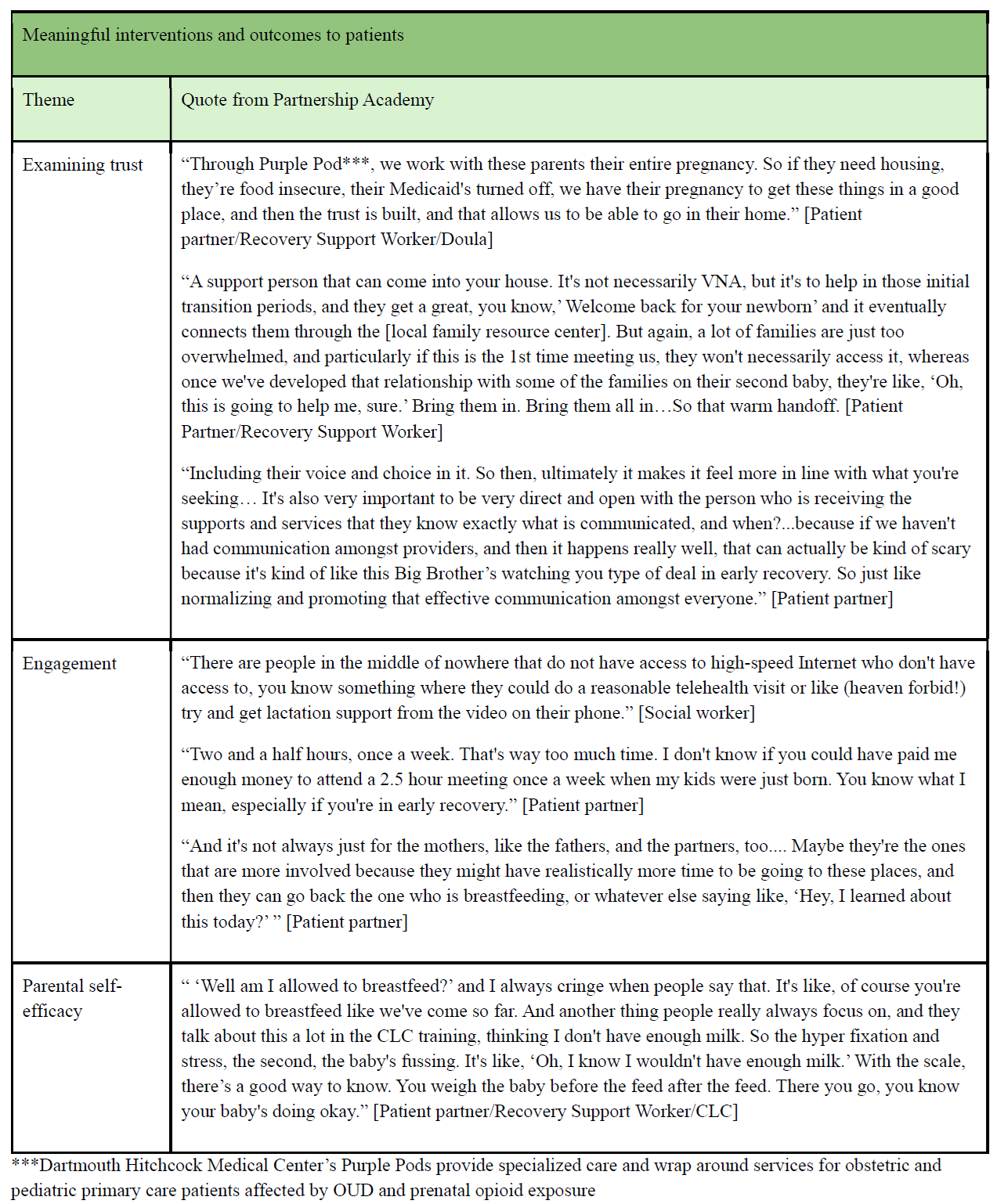
Results: Key elements to support a BF intervention identified include telehealth and remote engagement opportunities (e.g text messaging), promotion of continuity of care, PCP confidence in delivering care for OEN and their families, building on trusted relationships and integration of lived experience expertise. Significant barriers identified include provider and system-level biases, educational gaps, internalized stigma, limited household/community support, competing time demands and lack of internet access. Intervention outcomes meaningful to patients included examining trust, engagement, and parental self-efficacy.
Conclusion(s): Patient-generated information supports development of sustainable interventions. Leveraging telehealth BF support and continuity of care alongside community-based relationships fosters engagement. Gaps in knowledge, comfort and connection to resources at both patient and system levels present potential barriers. Next steps include co-designing targeted interventions, such as centralized resources to enhance culturally responsive and community connected care, building support networks for parental self-efficacy, and enhancing accessible telehealth options. Future work will explore tailored strategies to strengthen intervention components and ensure the needs of rural families post-delivery are effectively met.
Table 1: Identified Key Facilitators- Select Quotes
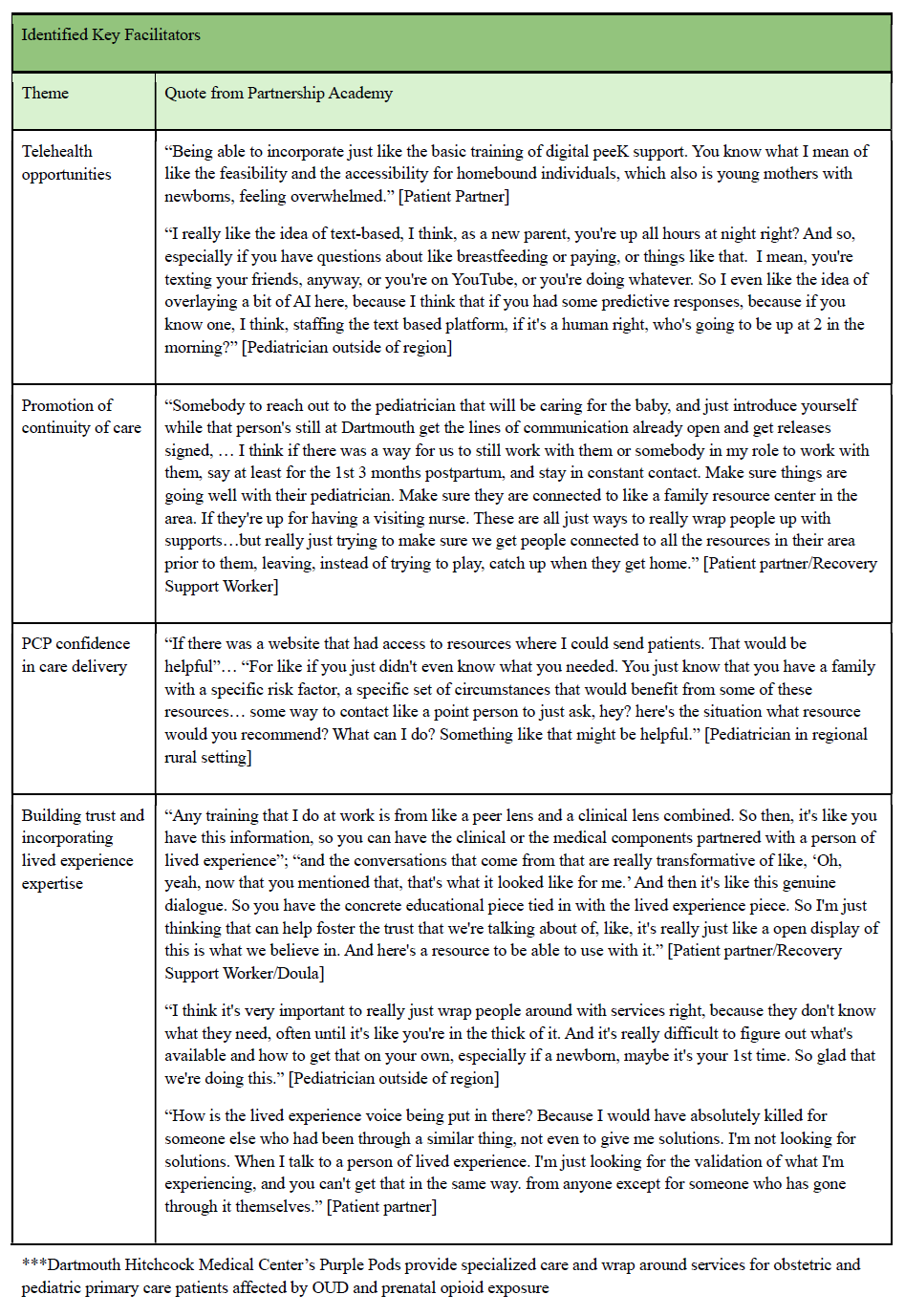
Table 1: Identified Barriers- Select Quotes
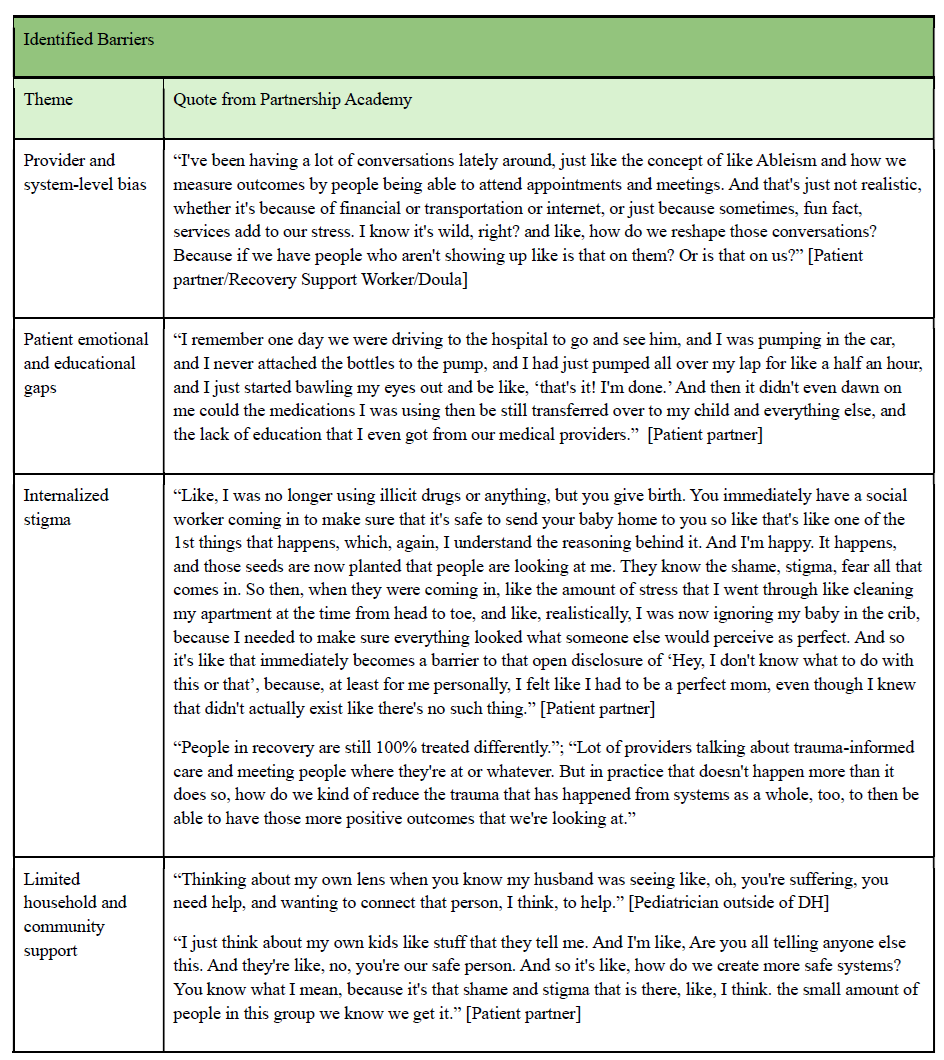
Table 3: Meaningful Interventions and Outcomes- Select Quotes