Health Equity/Social Determinants of Health 6
Session: Health Equity/Social Determinants of Health 6
733 - One Size Does Not Fit All: Comparing Socioeconomic Indices for Predicting Mortality After Heart Surgery
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 733.6014
Rittal Mehta, Childrens National Hospital, Washington DC, DC, United States; Alyssia Venna, Children's National Health System, Washington, DC, United States; Mitchell C. Haverty, Children's National Health System, Washington, DC, United States; Yves d'Udekem, Children's National Health System, Washington, DC, United States; Jennifer Klein, Children's National Health System, Washington, DC, United States
- RM
Rittal Mehta, MPH (she/her/hers)
Senior Research Scientist
Childrens National Hospital
Washington DC, District of Columbia, United States
Presenting Author(s)
Background: Socioeconomic status (SES) is a crucial determinant of health outcomes in children with congenital heart disease (CHD).
Objective: This study aims to compare the predictive capabilities of three SES indices—Social Deprivation Index (SDI), Distress Community Index (DCI), and Child Opportunity Index (COI)—in assessing overall mortality in a pediatric CHD cohort.
Design/Methods: We conducted a retrospective analysis of 2,546 patients. Neighborhood SES was categorized using the COI, resulting in three groups: disadvantaged (48.5%, n=1,235), moderate (20.6%, n=524), and advantaged (30.9%, n=787). This classification enabled direct comparison of the predictive performance of the COI, SDI, and DCI in assessing mortality risk. Multivariable logistic regression models, adjusted for key clinical and demographic variables (e.g., stat category, syndromes, chromosomal abnormalities), were used to identify predictors of mortality. Variable importance analysis highlighted the most influential predictors.
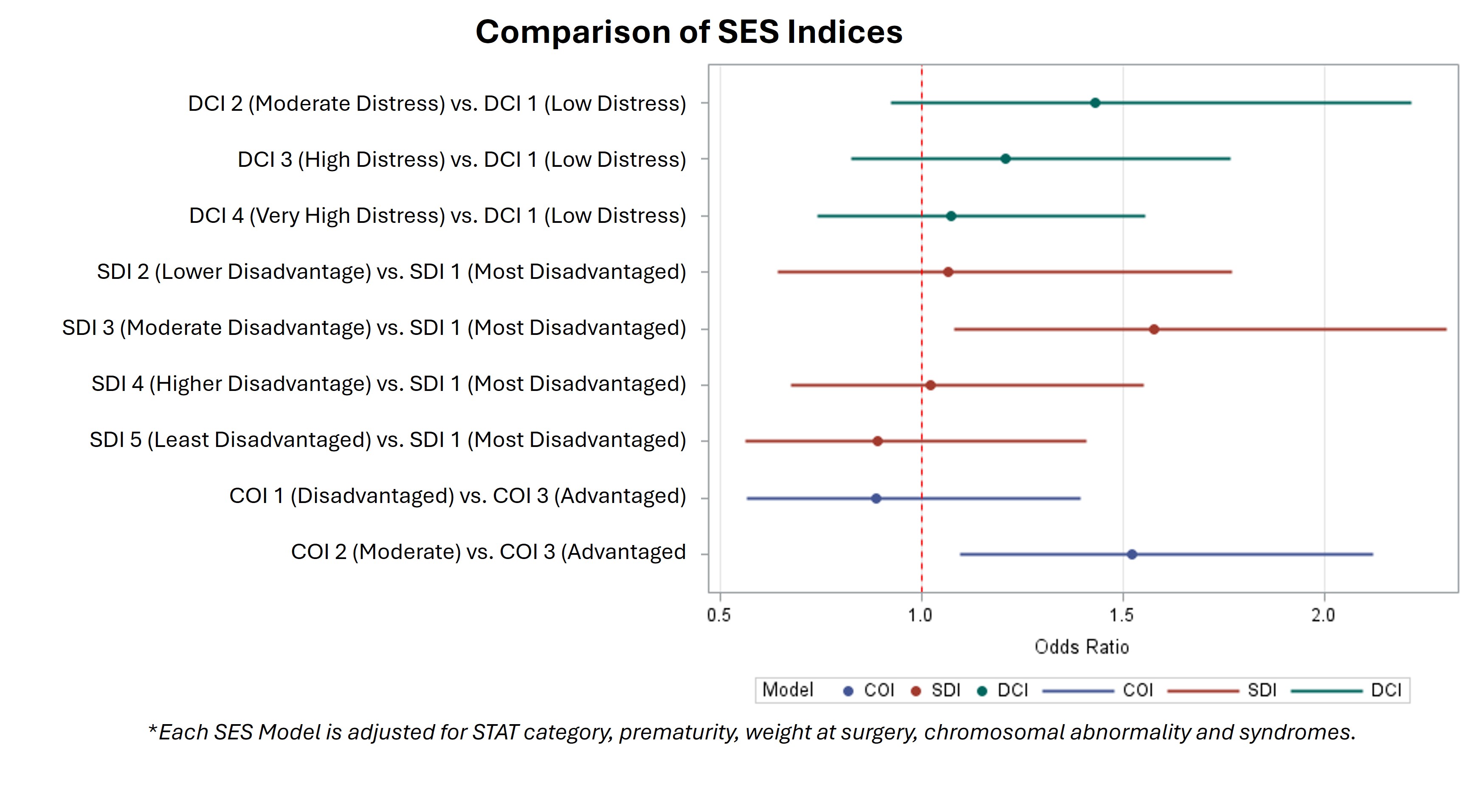
Results: Demographics of the study cohort (Table 1) reveal disparities in long-term mortality, with a 13.6% (n=168) rate for patients from disadvantaged neighborhoods vs. 8.4% (n=66) for advantaged (p < 0.001). Multivariable analysis showed a 1.524-fold increase in mortality risk for patients from disadvantaged areas. The COI model had the highest c-index of 0.80, while the SDI and DCI models had c-indices of 0.78 and 0.68, respectively. The SDI index model showed an OR of 1.67 (95% CI: 0.64-1.77) for the highest disadvantage category, while the DCI model showed an OR of 1.43 (95% CI: 0.925-2.217) for disadvantaged individuals, linking socioeconomic disadvantage to increased mortality risk (Figure 1). Other clinical factors, such as STAT category (OR = 6.588), premature birth (OR = 1.73), and genetic syndromes (OR = 1.61), also impacted mortality risk. SES indices contributed 14% to the model, underscoring their critical role in assessing health outcomes in pediatric congenital heart disease.
Conclusion(s): The COI model showed superior predictive performance for mortality in CHD patients, suggesting its clinical utility. The limited impact of the SDI and DCI indicates these measures may not fully capture urban mortality risk complexities. The absence of patients with the highest DCI score (DCI = 5) in Washington, DC, emphasizes the need for region-specific SES measures to address local disparities. Our findings highlight the importance of integrating socioeconomic considerations into clinical care and call for more research on SES indices' impact across diverse geographic settings.
Demographics and clinical characteristics of patients undergoing surgery after diagnosed with congenital heart disease
.jpg)
Comparison of SES Indices among patients undergoing surgery for congenital heart disease