Palliative Care
Session: Palliative Care
431 - Opportunities for Solid Organ Donation in the Neonatal Intensive Care Unit
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 431.5991
Sarah Pippin, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Ashley Sherman, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Julie Weiner, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Jotishna Sharma, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States

Sarah Pippin, MD (she/her/hers)
Pediatric Resident
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background: Pediatric patients are at an increased risk of mortality when waiting for an organ transplant. Approximately 50% of pediatric patients wait for > a year for a solid organ transplant and infants < 1 year of age have the highest death rate while awaiting transplantation. There are two pathways for organ donation (OD), donation after death by neurologic criteria (DDNC) or donation after circulatory determination of death (DCDD). Neonates rarely meet brain death criteria, and since most deaths in the NICU occur after a planned extubation, DCDD with organ procurement after a planned extubation from mechanical ventilation can be a consideration especially with kidney and liver donations. Organ procurement may be limited by warm ischemic time (WIT); usually ≤ 90 minutes. The question remains which neonates would meet criteria for DCDD.
Objective: The aim of this study is to characterize eligibility for donation after circulatory determination of death in infants undergoing withdrawal of care in the NICU based on WIT ≤ 90 minutes.
Design/Methods: Retrospective study of a cohort of infants ≥36 weeks at the time of death who died at a level IV NICU from January 1, 2012, to December 31, 2022. Demographic information was obtained. Mode of death was categorized as withdrawal of care, withholding of care, or CPR. The withdrawal of care was further examined for eligibility for DCDD based on WIT ≤ 90 minutes.
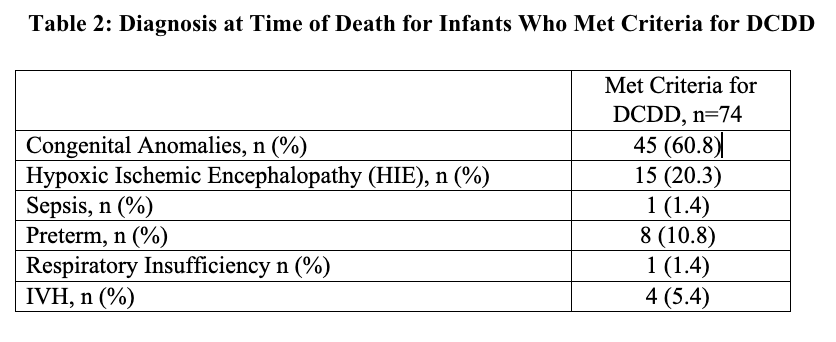
Results: During the study period, there were 337 infants ≥ 36 weeks at the time of death and of those, 67% (226/337) infants had withdrawal of care. The most common cause of death was congenital anomalies. Those who met DCDD criteria were found to have significantly higher birth weight (p= < 0.01), older GA at birth (p=0.01), and older PMA at death (p= < 0.01) Table 1. Table 2 shows the diagnosis at time of death for infants who met criteria for DCDD.
Conclusion(s): One third of NICU deaths ≥36 weeks undergoing withdrawal of mechanical ventilation could be potential solid organ donors after DCDD with WIT ≤ 90 minutes. Increased organ donation opportunities in this age group could have an impact on pediatric patients waiting for an organ transplant. Establishing a DCDD protocol in level IV NICUs should be strongly considered. Further studies are needed to determine factors that predict success of neonatal solid organ donation through DCDD.
NICU Deaths ≥ 36 weeks with Withdrawal from Mechanical Ventilation
.png)
Diagnosis at Time of Death for Infants Who Met Criteria for DCDD