Children with Chronic Conditions 2
Session: Children with Chronic Conditions 2
511 - Enhancing Primary Care Provider Knowledge of Cerebral Palsy Utilizing a Virtual Education ECHO Platform
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 511.5075
Nicole Jewett, Nationwide Children's Hospital, Columbus, OH, United States; Laurie Glader, Nationwide Children's Hospital, No concerns, OH, United States

Nicole Jewett, MD (she/her/hers)
Pediatric Resident PGY III
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Individuals with cerebral palsy (CP) require multi-specialty care for surveillance and management of co-morbidities associated with their underlying diagnosis. An increasing number of academic centers provide comprehensive CP programs to meet this need. However, for many patients, access to such programs is limited by geographic proximity. Instead, they depend on primary care professionals (PCPs) for monitoring, who often report a deficit in their CP knowledge. Project ECHO (Extension for Community Healthcare Outcomes) provides a virtual platform that facilitates specialty education and support to medical professionals via didactic and case-based presentations and creates a unique opportunity to address this CP knowledge gap.
Objective: To leverage the ECHO model to improve PCP knowledge and confidence in caring for children with CP.
Design/Methods: A team of physicians, therapists and parents with expertise in CP created and delivered an eight-session videoconference curriculum to a group of 46 self-selected PCPs, trainees and professionals dedicated to childhood onset disability. Each session included a didactic presentation followed by discussion and a relevant attendee-presented case. Pre/post- surveys were administered to assess clinician knowledge and self-efficacy.
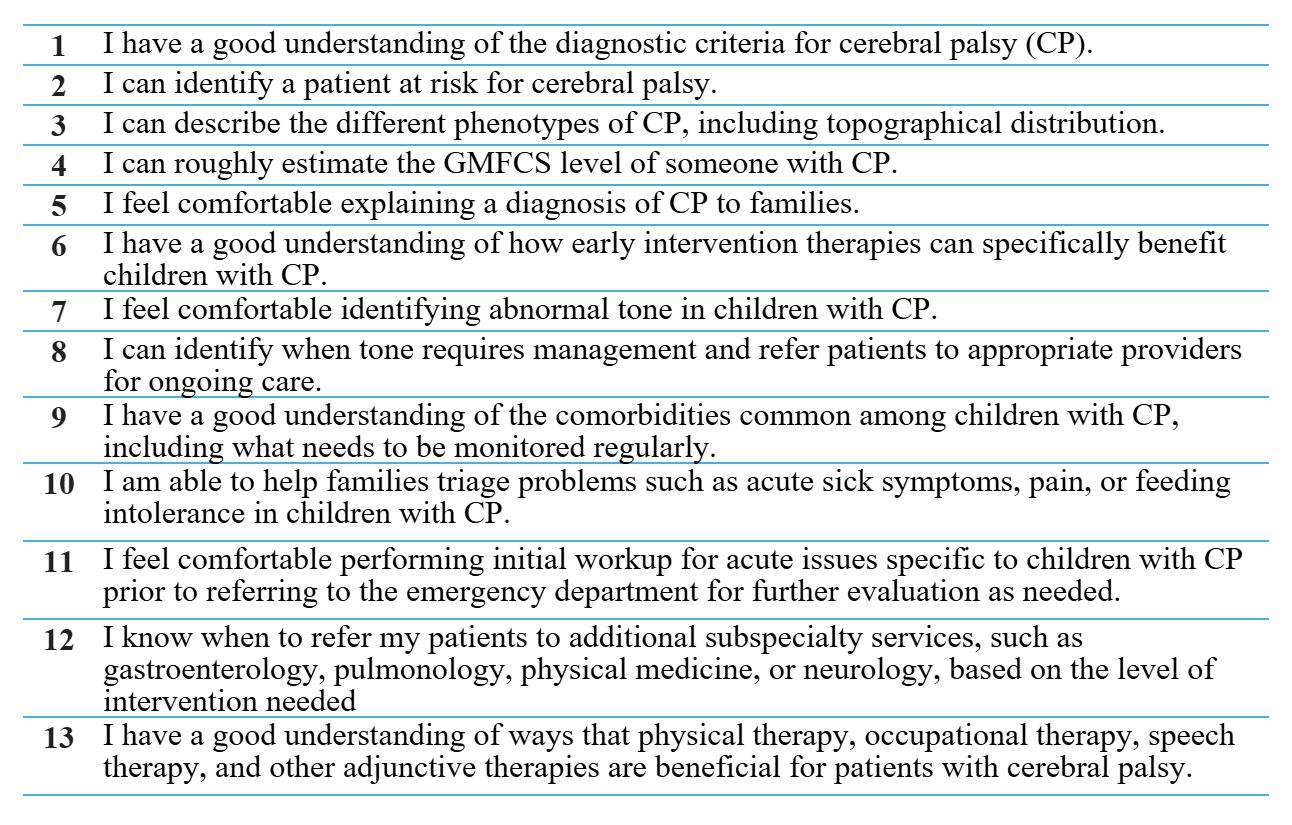
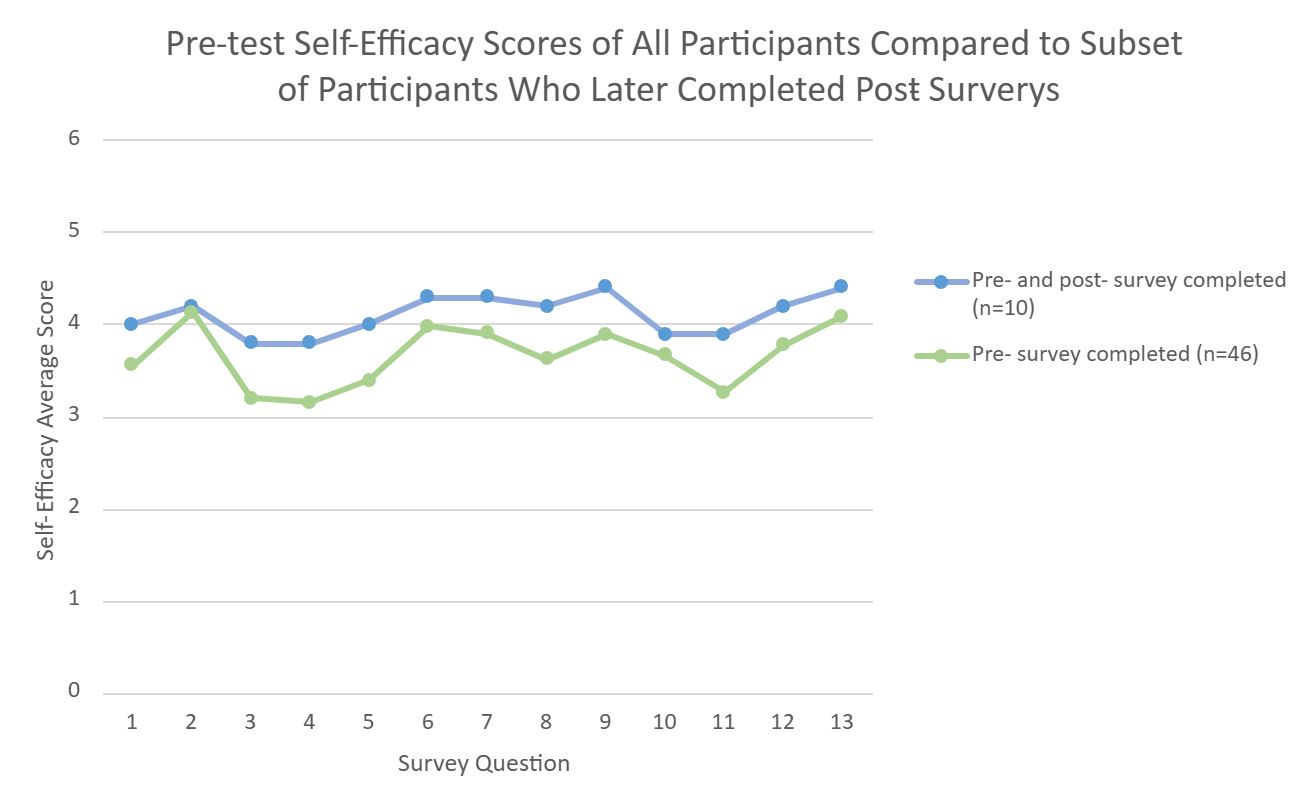
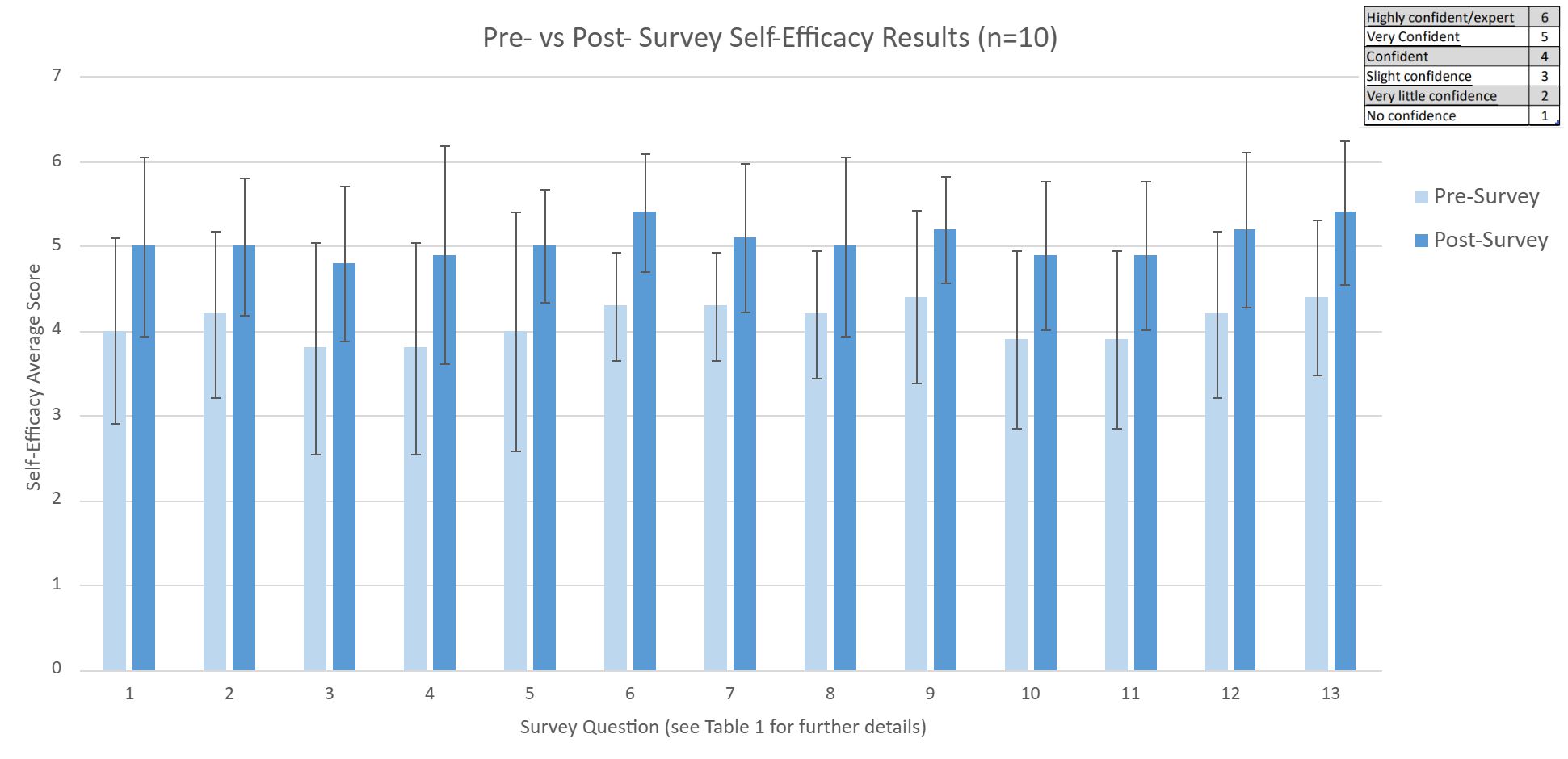
Results: Attendance varied between 11–27 participants per session. 33 (72%) attendees were physicians or nurse practitioners. Pre-survey findings of all 46 participants suggested room for knowledge enhancement. Over 90% of attendees ranked all didactics as providing useful information likely to change clinical practice. Participants anticipated changes such as referring earlier to therapies, prioritizing nutritional needs, and utilizing frequent mental health assessments. Ten (22%) attendees completed full pre- and post- surveys; those who completed both had a higher knowledge base prior to the series (Figure 1). Findings indicate statistically significant (p < 0.05) improvement in knowledge and confidence across all assessed fields (Figure 2 and Table 1).
Conclusion(s): The ECHO model provides a feasible virtual opportunity to boost PCP knowledge and comfort in managing children with CP. Data was gathered from participants who, based on the pre-survey analysis, were relatively knowledgeable in treating children with CP. Although sample size was small, results signal the efficacy of providing education even to those already confident in CP management. Further study with larger sample sizes will clarify impact, including assessment of the meaningful outcome of practice change.
Figure 1:
 Initial knowledge base as evidenced by pre-test self-efficacy scores was higher among the ten participants who completed both pre- and post-surveys compared on average to total 46 attendees.
Initial knowledge base as evidenced by pre-test self-efficacy scores was higher among the ten participants who completed both pre- and post-surveys compared on average to total 46 attendees. Figure 2:
 Improvement in self-efficacy scores after completing ECHO CP series.
Improvement in self-efficacy scores after completing ECHO CP series. Table 1: Survey Questions