Hospital Medicine 4: Medical Education
Session: Hospital Medicine 4: Medical Education
159 - Interdisciplinary Perspectives on Clinical Leadership of Inpatient General Pediatric Teams: A Multi-Institutional Qualitative Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 159.5350
Elizabeth Nguyen, Lucile Packard Children's Hospital Stanford, Mountain View, CA, United States; David Mahoney, Seattle Children's, Seattle, WA, United States; Peggy Han, Stanford University School of Medicine, Palo Alto, CA, United States; Tracy Seimears, Seattle Children's, Seattle, WA, United States; Nicole R. Washington, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Sara Singer, Stanford University School of Medicine, Stanford, CA, United States; Sarah Hilgenberg, Stanford, Palo Alto, CA, United States

Elizabeth Nguyen, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Lucile Packard Children's Hospital Stanford
Mountain View, California, United States
Presenting Author(s)
Background: Leadership in clinical settings impacts quality of patient care, team members’ job satisfaction, and trainees’ perceived learning environment. Yet, medical training often lacks structured leadership development. Hackman’s Model of Team Effectiveness outlines 5 conditions leaders establish to promote team effectiveness, defined as achieving performance goals and team and individual growth. Published physician leadership competencies reflect program directors' and attendings' views, but not other members of patient care teams whose perspectives on effective leadership are essential to understand.
Objective: To explore the meaning of CL for interdisciplinary providers on inpatient general pediatric (IGP) teams, develop a conceptual model of CL in this context, and identify effective leadership behaviors described by participants.
Design/Methods: In this IRB-exempt study, we used a constructivist grounded theory approach and conducted semi-structured interviews of interdisciplinary team members (attendings, residents, nurses, allied health providers) at 3 large, geographically diverse, university-based children’s hospitals. We employed stratified sampling with a maximum variation approach to capture diverse perspectives across roles, career experience, and demographics, intentionally amplifying underrepresented voices. All research team members participated in coding; two independently coded each transcript using deductive and inductive methods.
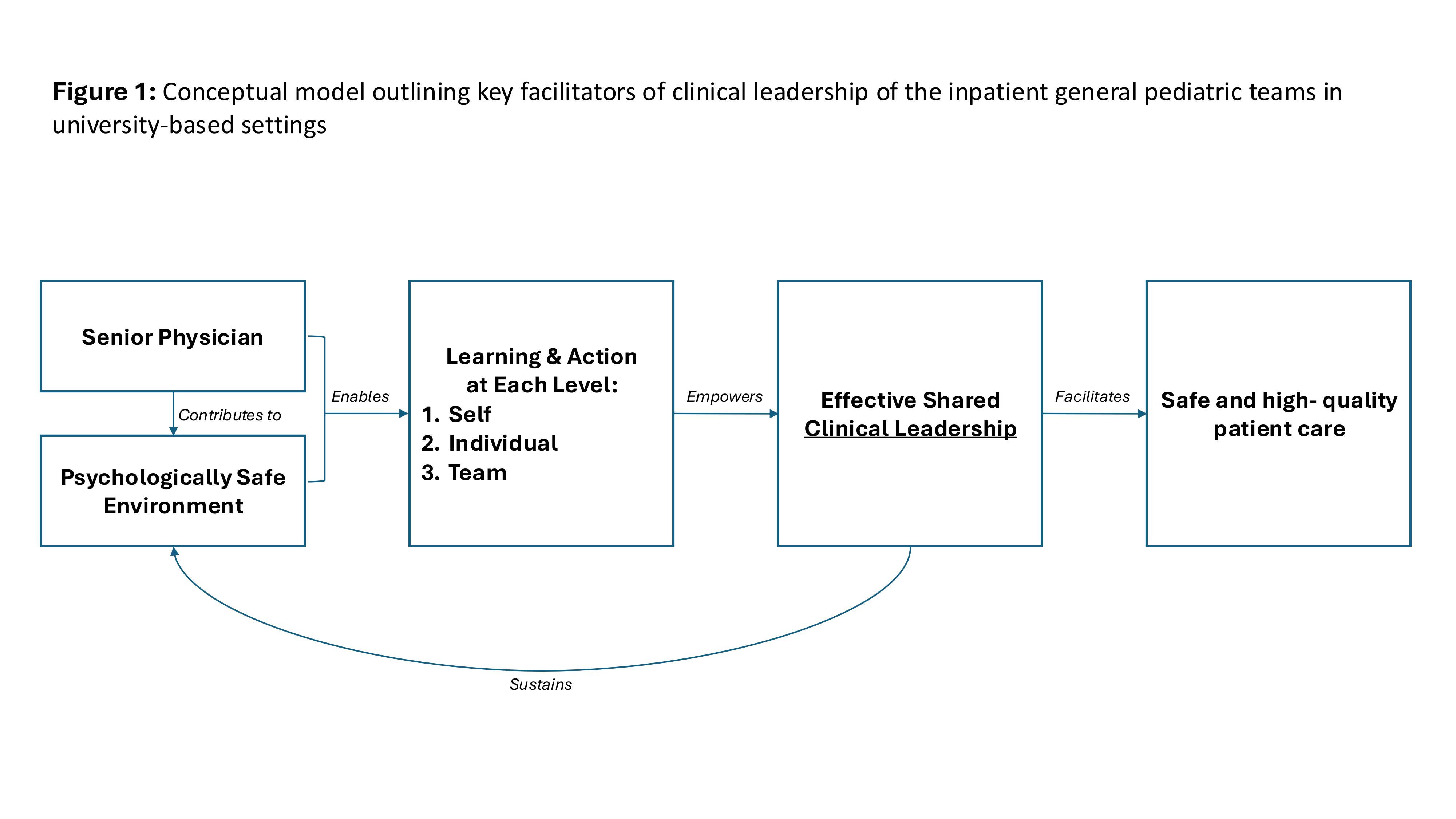
Results: We conducted 26 interviews across institutions and roles. Participants expressed that CL of IGP teaching teams is shared across roles and hierarchy. This shared leadership is fostered by a supportive senior physician (SP) (attending, senior resident) and a psychologically safe environment, enabling learning and action at multiple levels: self, individual team members, and the team as a whole. By engaging each level, SPs empower team members to share in CL responsibility, which mobilizes them to deliver safe, high-quality patient care [Figure 1]. Participants identified that SPs enable CL at all levels by contributing to a psychologically safe environment, establishing clear direction and expectations, promoting autonomy, and integrating teaching. They also noted that effective CL across all roles requires strong communication and collaboration.
Conclusion(s): In IGP settings, CL is shared interprofessionally and across hierarchy. SPs and team members can effectively optimize CL by demonstrating modifiable behaviors that can potentially enhance the learning environment, foster a positive culture, and improve patient care on IGP teaching teams.
Figure 1: Conceptual model outlining key facilitators of clinical leadership of the inpatient general pediatric teams in university-based settings