Children with Chronic Conditions 1
Session: Children with Chronic Conditions 1
496 - High Intensity Care Management for Children with Medical Complexity and High Social Needs
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 496.5371
Erin Avondet, University of Utah School of Medicine, Salt Lake City, UT, United States; Adriana Martinez, Primary Children's Hospital, Herriman, UT, United States; Carolyn Reynolds, Intermountain Healthcare, Salt Lake City, UT, United States; Laura Holden, University of Utah School of Medicine, South Jordan, UT, United States; Karine Romero, Primary Children's Hospital, SLC, UT, United States

Erin Avondet, MD (she/her/hers)
Assistant Professor of Pediatrics
University of Utah School of Medicine
Riverton, Utah, United States
Presenting Author(s)
Background: Children with medical complexity and their families are particularly susceptible to the impacts of unmet social needs. In addition to higher healthcare utilization, the literature describes higher rates of poverty, food and housing instability, economic risk, and more. In response to these concerns, Intermountain Primary Children’s Hospital developed an intensive care management program to partner with families to address social determinants of health (SDOH) and care access issues via hands-on assistance with resources, intensive care management, and patient education.
Objective: To provide intensive care management to children with medical complexity to address social and medical needs impacting health and healthcare access
Design/Methods: Patients living in Salt Lake County with high medical complexity (3 body systems or more) and SDOH affecting healthcare access were eligible for enrollment. Team members administer validated screening tools upon enrollment to evaluate for social needs affecting child health and wellbeing. Over the course of enrollment, team members work to address SDOH through hands-on assistance and in-home visits while being inclusive of the family’s abilities, culture and language, and dynamics. In addition to addressing SDOH, the team worked to create points of contact for families within the community and medical system to maximize outpatient support and avoid unnecessary hospital utilization.
Results: Over the life of the program, over 140 patients have been enrolled in our services, with an average active census of 28 patients. Chart review shows 45% of all patients are non-English preferring (Table 1). A majority of patients live in Very Low or Low Child Opportunity Index (COI) zip codes (Table 2). The most common social needs reported by families were clothing, living space, and ability to pay bills. Data collected over the course of the program has shown an average 53% reduction in hospital admissions and a steady reduction in ED visits (a 28% reduction) when comparing pre- and post-enrollment data (Table 3).
Conclusion(s): The Connector Service Program demonstrates the value of high intensity care management to address SDOH and provide medical support to patients marginalized by medical and social systems. By connecting families with community resources and medical systems, we can empower them to overcome barriers and navigate challenging and inequitable systems while helping medically complex children to grow and thrive in their homes. Further evaluation is needed to understand the team's impact on social and medical needs and ongoing improvement strategies for our approach.
Table 1
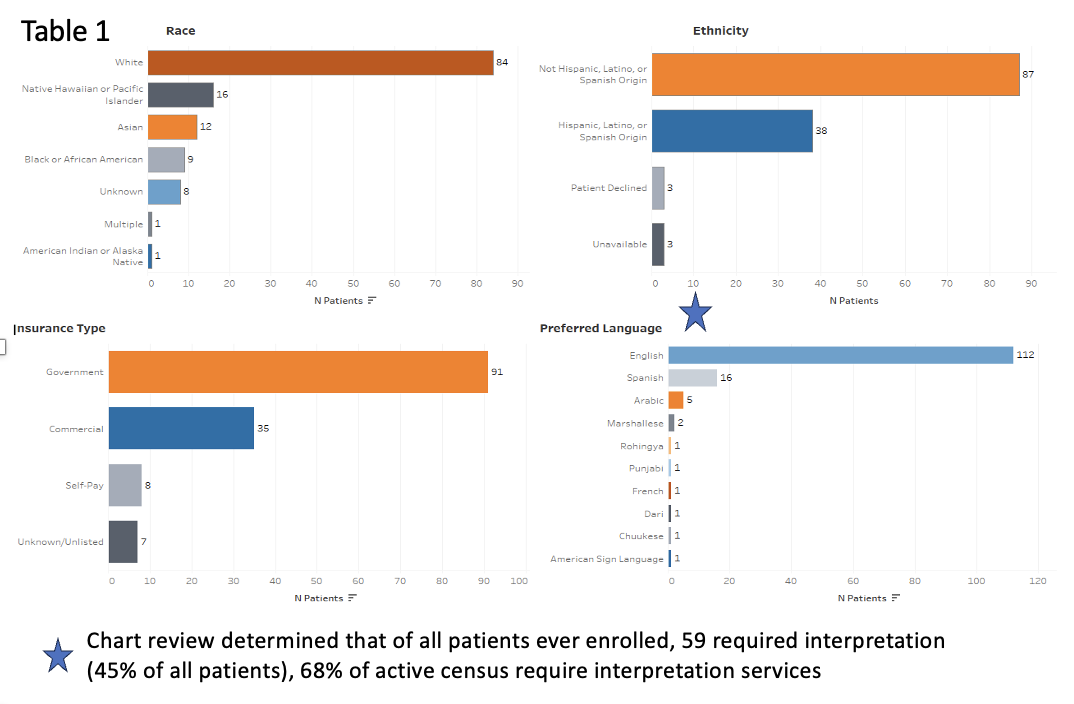 Connector Service patient demographic information
Connector Service patient demographic informationTable 2
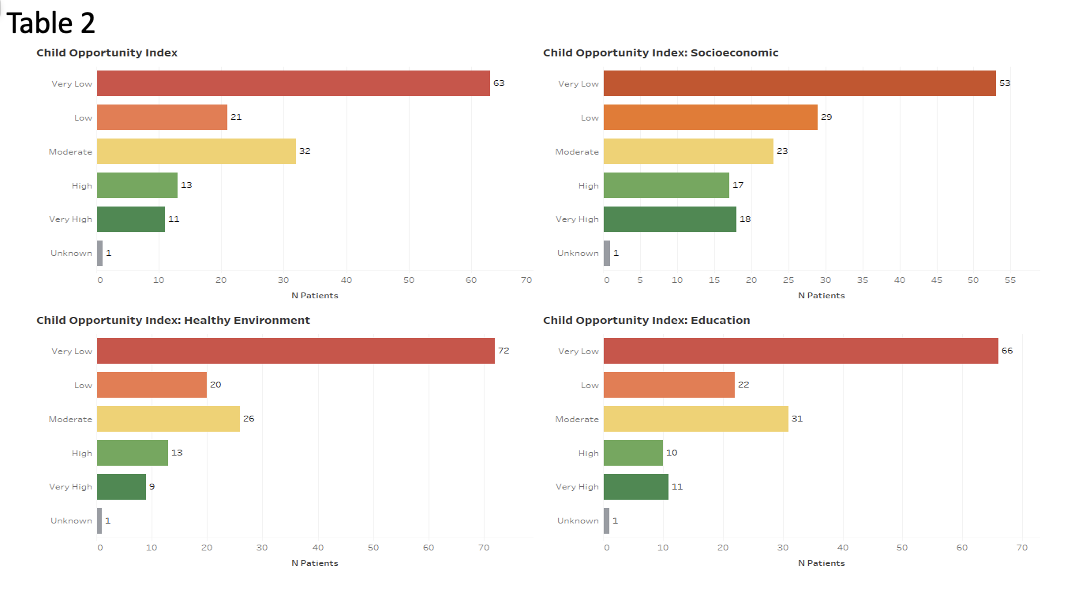 Connector Service patient COI distribution
Connector Service patient COI distributionTable 3
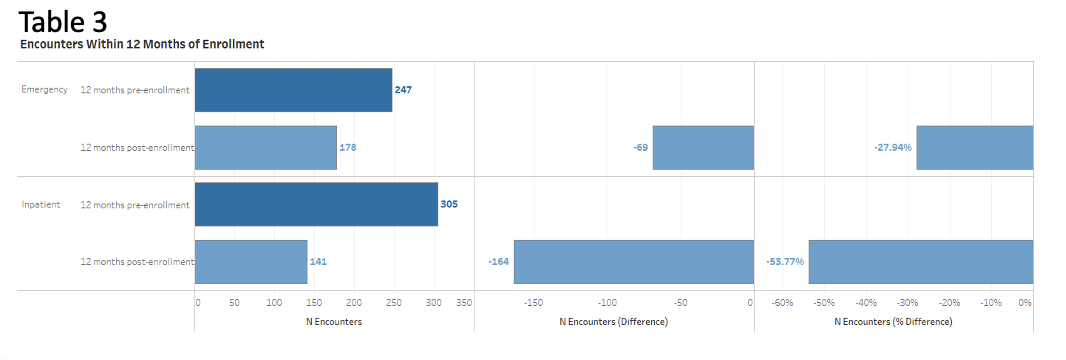 Connector Service hospital utilization data
Connector Service hospital utilization data
