Obesity 2
Session: Obesity 2
288 - Health behavior influences for 18-26 year olds with prediabetes: A qualitative study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 288.5367
Abigail Arons, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Mai Baalbaki, University of California, San Francisco, Berekeley, CA, United States; Amy Beck, University of California, San Francisco, School of Medicine, San Francisco, CA, United States
- AA
Abigail Arons, MD MPAff (she/her/hers)
Fellow, National Clinician Scholars Program
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Nearly a quarter of older adolescents and young adults (AYA) have prediabetes yet lifestyle interventions are less effective in this age group than for older and younger patients. Establishing healthy diet and physical activity behaviors is especially important in this age group as these behaviors carry forward throughout adulthood. While prior studies elicited older AYA perspectives on behavior change for weight loss, we hypothesize that older AYAs with prediabetes may have unique behavioral drivers in the context of preventing diabetes.
Objective: To understand perspectives of older AYA with prediabetes on the individual and external factors that influence their diet and physical activity behaviors.
Design/Methods: We conducted semi-structured interviews in English and Spanish with outpatients ages 18-26 with prediabetes (HgbA1c or chart diagnosis) from January to September 2024, at one safety net hospital and one academic medical center. The interviews addressed current health behaviors and barriers and facilitators to health behavior change to reduce diabetes risk and were informed by the Capability-Opportunity-Motivation-Behavior (COM-B) framework. We determined themes using thematic analysis.
Results: We interviewed 24 participants (63% female, 71% Latino/a/x, 29% Black, 61% food insecure, 39% any college, mean age 22.6). Participants reported relatively high Capability: Health knowledge was sophisticated, with interviewees understanding prediabetes and healthy eating, citing learning with school health and nutritionists. In contrast, we found major Opportunity barriers, with numerous external factors presenting critical challenges including high social needs, low control over time, tension in independence from family, and neighborhood environments that make change difficult. Motivation was variable: one subgroup with a growth mindset felt motivated to avoid diabetes whereas another subgroup felt less optimistic. (Tables 1-3)
Conclusion(s): Our participants reported high levels of pre-existing Capability with regards to lifestyle change, yet struggled to translate their knowledge into healthy behaviors. One clear need is support in overcoming Opportunity barriers (e.g. social and economic needs, psychosocial connection, negative environmental influences). Further, there may be two distinct subgroups of older AYA with prediabetes with different intervention needs (one with high motivation but requiring additional resources, versus one with lower motivation requiring encouragement). Future work is needed to quantify these findings and co-design responsive diabetes prevention interventions for older AYA.
Table 1. Interview themes with example quotes, in the Capability domain
.jpg)
Table 2. Interview themes with example quotes, in the Opportunity domain
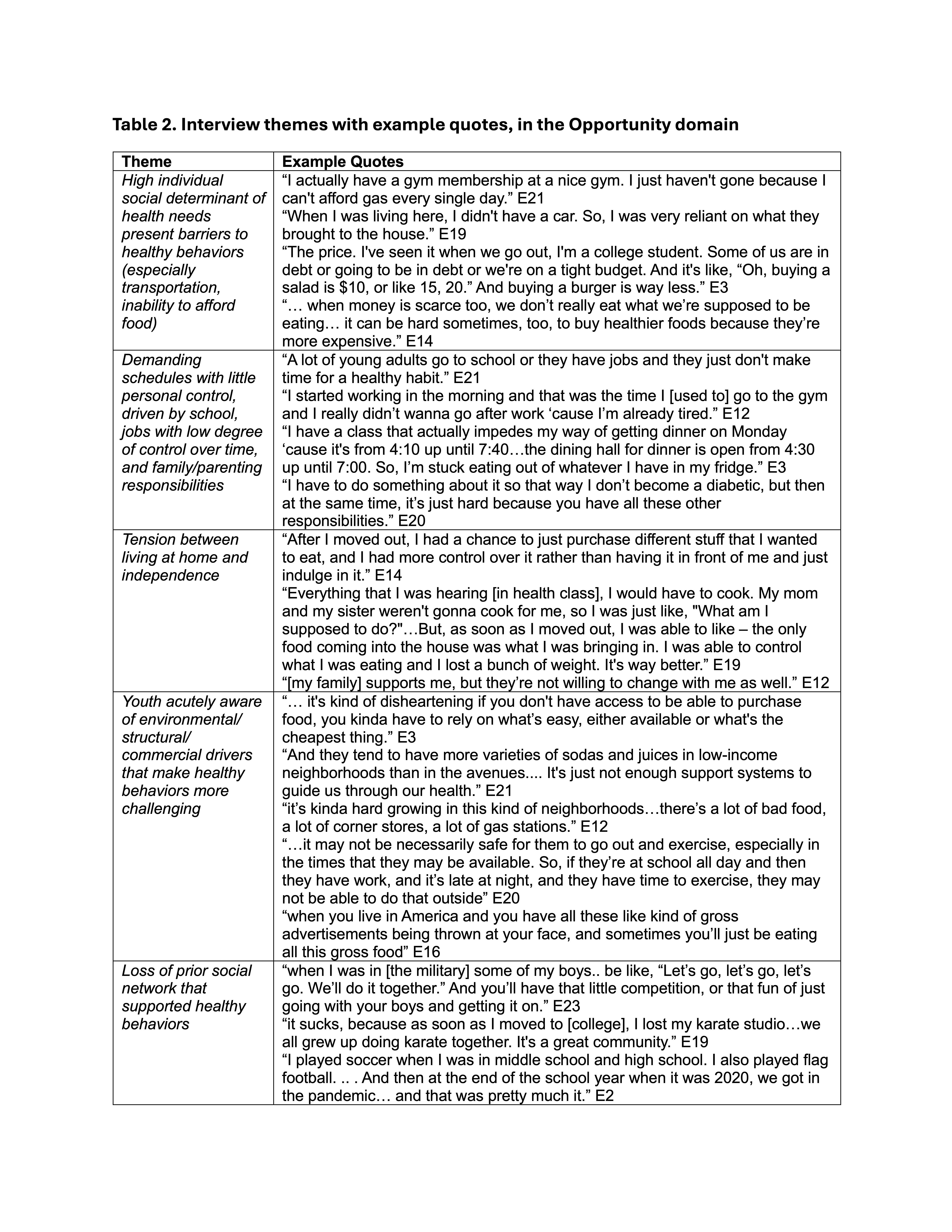
Table 3. Interview themes with example quotes, in the Motivation domain
.jpg)

