Child Abuse & Neglect 1
Session: Child Abuse & Neglect 1
344 - Implementation of an APP Certification and 24/7 In-Person Response Model for Child Abuse Pediatrics
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 344.5393
Angela L. Rabbitt, Medical College of Wisconsin, Milwaukee, WI, United States

Angela L. Rabbitt, DO (she/her/hers)
Professor of Pediatrics
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Up to 15.2% of US children experience child maltreatment, resulting in significant long-term impacts to health and well-being and an estimated national economic burden of >$100 billion per year. Accurate identification of maltreatment is critical to reduce short and long-term impacts and to use scarce resources wisely. Despite this, Child Abuse Pediatrics (CAP) has one of the lowest subspecialist to child ratios and lowest projected growth of all of the pediatric subspecialties. The CAP-trained medical workforce is insufficient, strained, and burning out. Advanced Practice Providers (APPs) can augment the CAP workforce as resiliency supporting team members, but rigorous training is important to ensure competent care in this legally charged specialty.
Objective: To develop and assess the impact of an APP certification program and 24/7 CAP in-person response model on provider workflows and engagement.
Design/Methods: Program leaders utilized national accreditation standards for APP residency and CAP fellowship training to create a 2-year comprehensive APP CAP certification program. The curriculum is integrated into clinical work, which includes rotating daytime, evening, night, and weekend call with in-person availability and protected time for scholarly activity and community engagement. Attendings provide oversight and create the final impression for hospital-based consults. Quarterly competency-based evaluations guide progressive independence and elicit trainee feedback about the curriculum. Surveys and listening sessions assessed external and internal stakeholder perceptions of program impact on patient care quality and subspecialty collaboration.
Results: The average length of time to independence was 10.8 months (range 9-14) on the outpatient service and 19.1 months (range 15-23) on the hospital-based service. APP trainees rated the training program good to excellent and emphasized the importance of graduated patient volume, mentoring, didactics, and peer review. Since program implementation, utilization of the hospital-based consult team overall has increased by 70%. Mean engagement scores for CAP providers increased 0.24 points (4.63 vs. 4.39 in 2023; 2024 mean industry percentile rank = 88th percentile). External partners and subspecialty colleagues perceive fewer disagreements and improved collaboration between pediatric subspecialists and higher quality patient care.
Conclusion(s): Expanding 24/7 access to highly trained APPs is an effective method to increase utilization of child abuse pediatrics expertise while also maintaining resilience and engagement of the child abuse pediatrics workforce.
Figure 1. Average encounters/month: Hospital-based CAP team
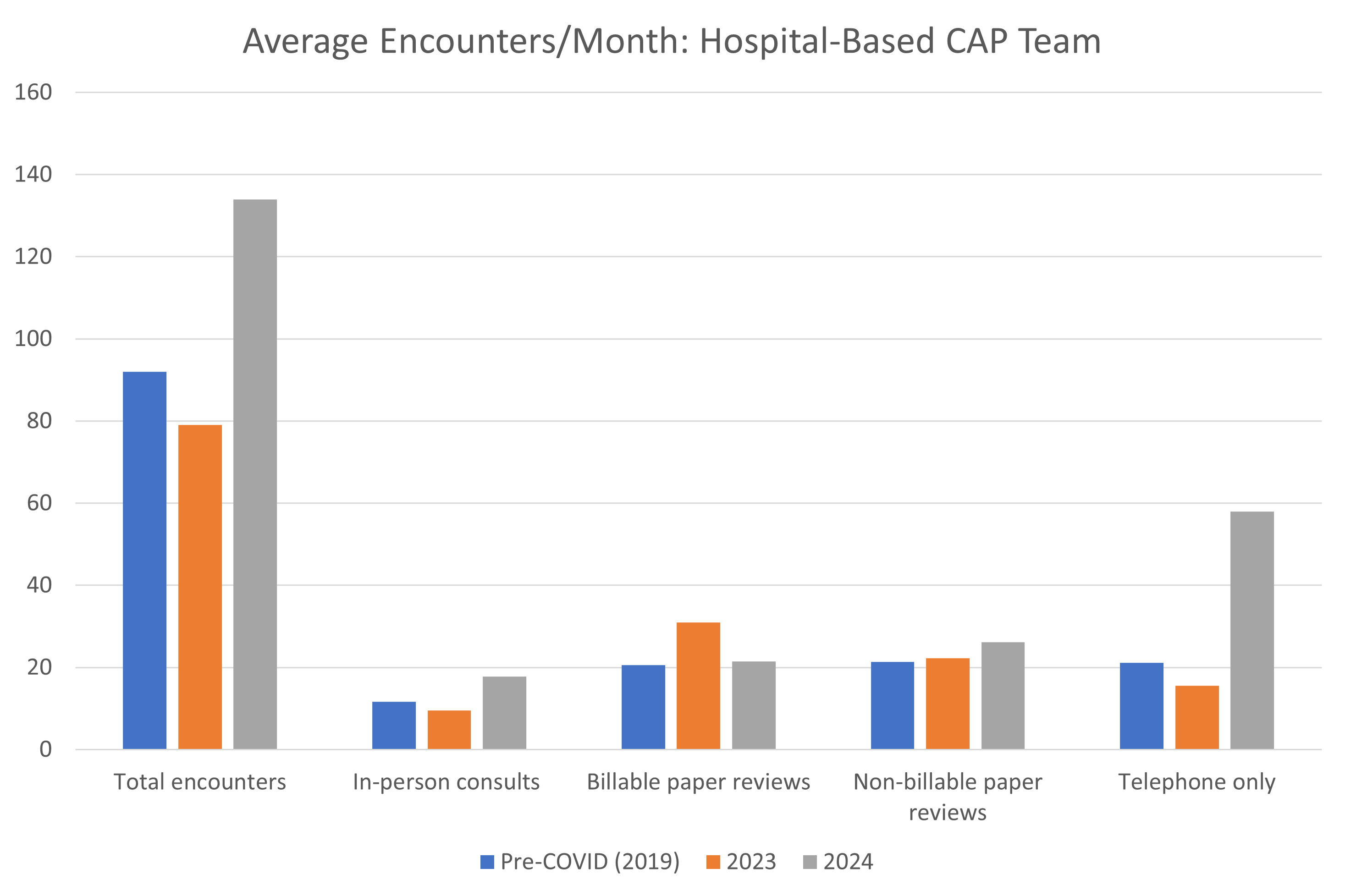 Total contacts to the hospital-based team increased by 70% in 2024 after implementation of 24/7 in-person availability in January 2024, with an 87% increase in in-person evaluations. Increases due to recovery of patient care volumes after the COVID pandemic do not fully account for the increase in patient care encounters.
Total contacts to the hospital-based team increased by 70% in 2024 after implementation of 24/7 in-person availability in January 2024, with an 87% increase in in-person evaluations. Increases due to recovery of patient care volumes after the COVID pandemic do not fully account for the increase in patient care encounters.Figure 2. 2024 Hospital-Based Encounters by Month
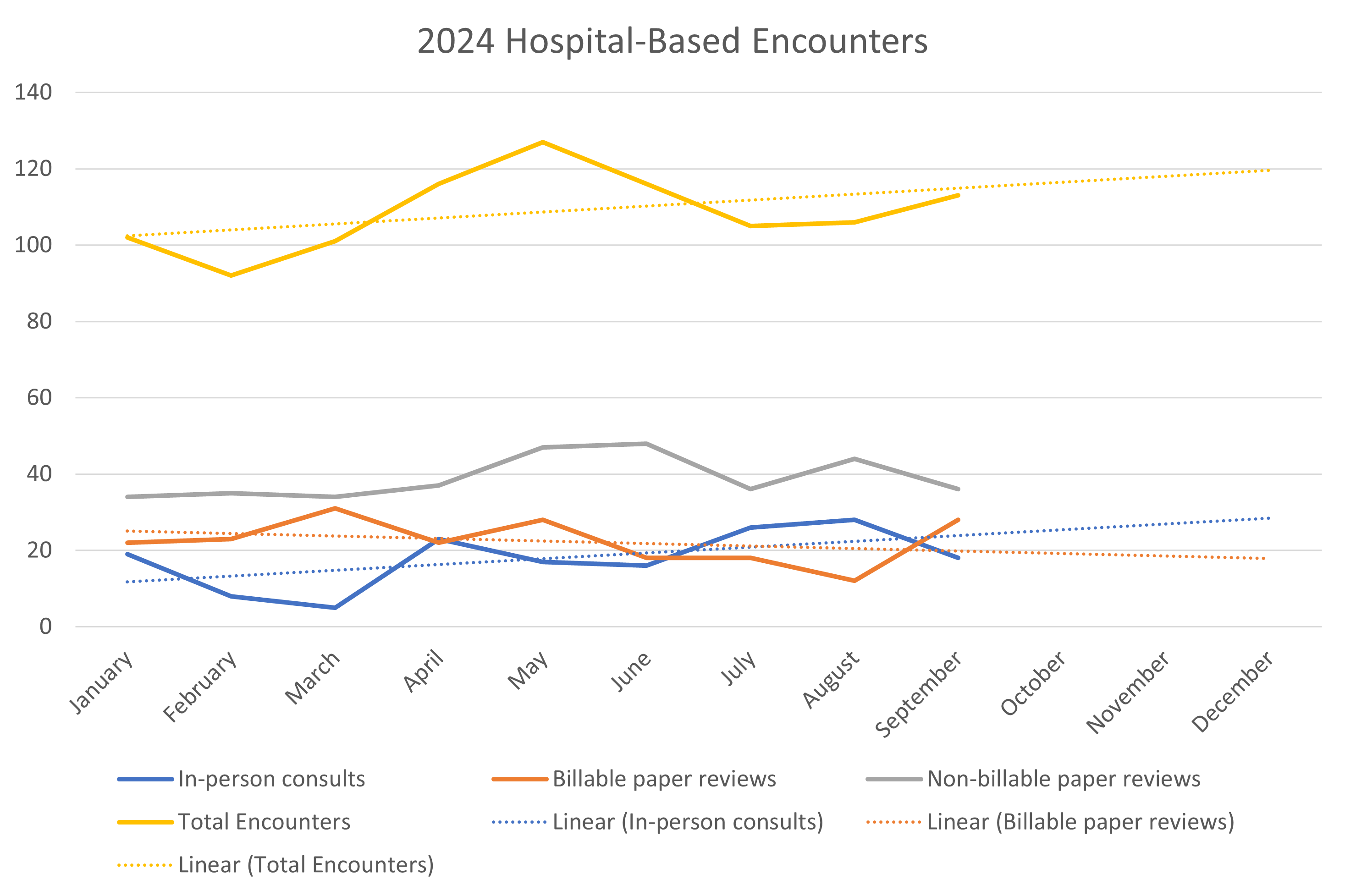 The volume of total hospital-based encounters and in-person consultations has steadily increased since implementation of the 24/7 in-person response model in January 2024 while the number of comprehensive (billable) paper reviews per month has decreased.
The volume of total hospital-based encounters and in-person consultations has steadily increased since implementation of the 24/7 in-person response model in January 2024 while the number of comprehensive (billable) paper reviews per month has decreased.
