Child Abuse & Neglect 1
Session: Child Abuse & Neglect 1
343 - Identifying Prior Concerning Injuries in Children with Abusive Fractures
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 343.5263
Noelle Tran, Children's Mercy Hospital, Kansas City, MO, United States; Maria C. Antonucci, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Angela Bachim, Baylor College of Medicine, Houston, TX, United States; Colleen J. Bressler, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Kristine A. Campbell, University of Utah School of Medicine, Salt Lake City, UT, United States; Nara Cho, Nationwide Children's Hospital, Columbus, OH, United States; Kristin G. Crichton, Nationwide Children's Hospital, Columbus, OH, United States; Lori Frasier, Penn state hershey, Hershey, PA, United States; Nancy S. Harper, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Sara Kilbride, Children's Mercy Hospitals and Clinics, kansas city, MO, United States; Natalie Laub, University of California, San Diego School of Medicine, San Diego, CA, United States; Jan Leonard, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Daniel Lindberg, University of Colorado Anschutz Medical Campus, Denver, CO, United States; Joanne N. Wood, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Jim Anderst, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States

Noelle Tran, DO (she/her/hers)
Pediatric Emergency Medicine and Child Abuse Pediatrics Fellow
Children's Mercy Hospital
Kansas City, Missouri, United States
Presenting Author(s)
Background: Existing data characterizes the relationship between prior concerning injuries (PCIs) in infants preceding abusive head trauma. Little data exists on the relationship between PCIs and abusive fractures.
Objective: We aim to compare the frequency and number of PCIs known to a Child Abuse Pediatrician (CAP) at the time of evaluation between children with abusive and non-abusive fractures.
Design/Methods: This was a retrospective, case-control study using data from CAPNET, a research network of 10 Child Protection Teams, over a 27-month period. Study subjects were less than 4 years old, had fractures, in-person CAP consultation, and did not have intracranial hemorrhage. The prevalence and number of PCIs was compared between abuse cases and non-abuse controls. Abuse was defined in two different ways to help mitigate circular reasoning. Analysis 1 compared the prevalence and number of PCIs among subjects with a score of 5-7 on a 7-point scale to identify likelihood of abuse cases to subjects with a score of 1-2. For Analysis 2, a combination of mobility, history, presence of concomitant suspicious injuries (CSIs), and fracture specificity for abuse were used a priori identify abused cases and controls. CSIs were defined as bruising and/or petechiae specific for abuse, subconjunctival hemorrhage outside of birth, burns, multiple fractures, fractures of different ages, and abdominal injury. Unadjusted odds ratios and 95% confidence intervals were calculated.
Results: There were 1339 study subjects with a median age of 8 months (interquartile range 3.8 to 13.9 months). The prevalence of PCIs in the abused groups in Analyses 1 and 2, respectively, were 30% and 22%. In Analysis 1, abused subjects had higher odds of any PCIs than the non-abused group (OR 4.5, 95% CI 3.2-6.1). This association remained in subjects with one (OR 3.4, 95% CI 2.4-4.9) and multiple PCIs (OR 11.7, 95% CI 5.8-23.8). In Analysis 2, any PCIs were also more common in immobile (OR 5.9, 95% CI 3.1-11.3) and mobile abuse group (OR 3.0, 95% CI 1.6 to 5.6) when compared to same level of mobility non-abuse groups. This association remained in immobile subjects with one (OR 5.1, 95% CI 2.5-10.4) and multiple PCIs (OR 9.5, 95% CI 2.2-40.0). Similarly, the association remained in mobile subjects with one (OR 2.1, 95% CI 1.1-4.0) and multiple PCIs (OR 33.3, 95% CI 1.9-572.6).
Conclusion(s): Children who suffered abusive fractures were more likely to have PCIs. This data supports the idea that abuse is commonly a chronic, escalating disease, and that improved early recognition has the potential to prevent significant injuries.
Table 1. Prevalence/type of prior concerning injuries by analysis
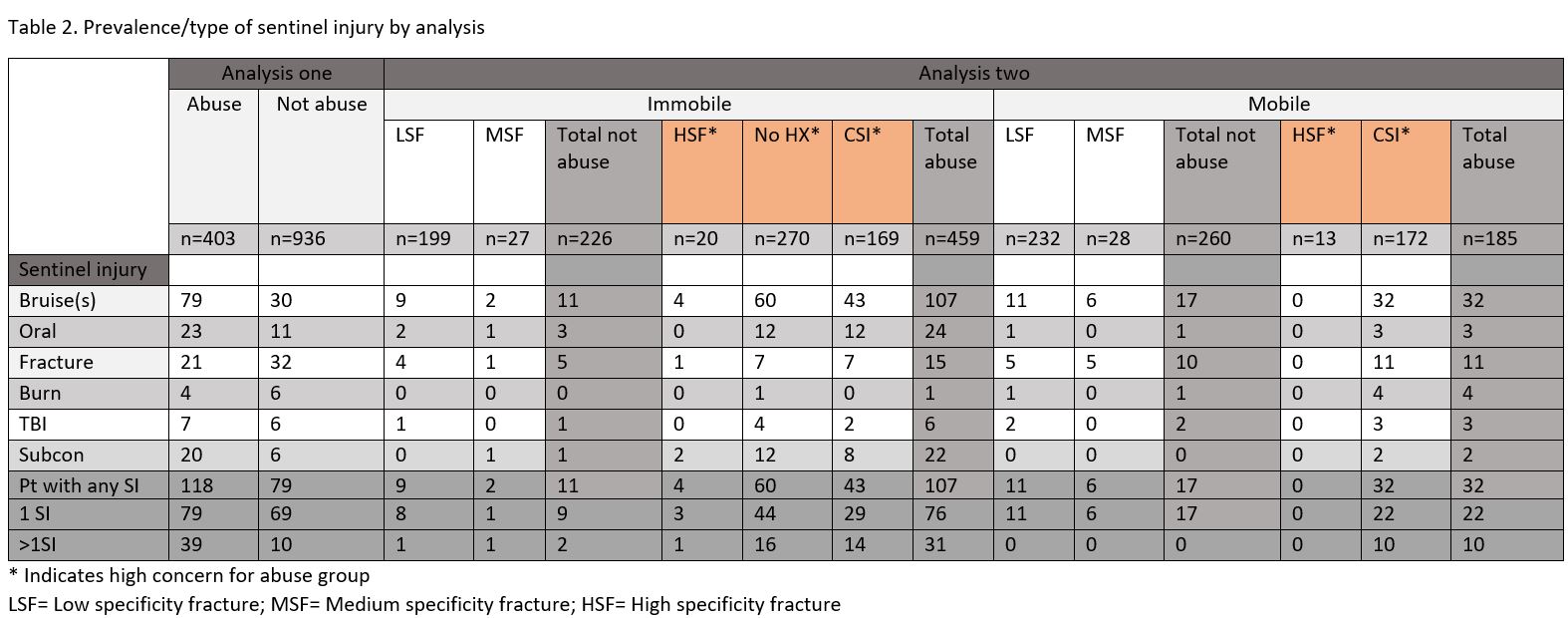 This table shows the prevalence and types prior concerning injuries found in each analysis
This table shows the prevalence and types prior concerning injuries found in each analysisFigure (1): Patient population separated into Analysis 1 and Analysis 2
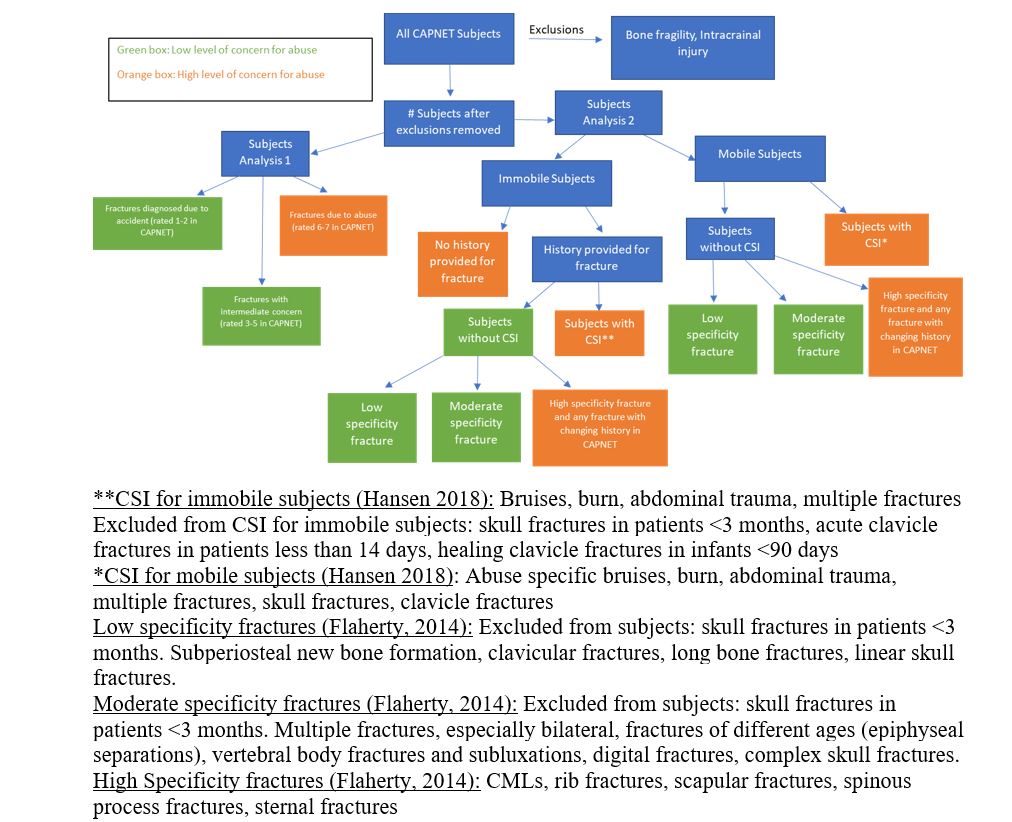 This table shows how the same patient population was separated into Analysis 1 and Analysis 2.
This table shows how the same patient population was separated into Analysis 1 and Analysis 2.
