Health Equity/Social Determinants of Health 4
Session: Health Equity/Social Determinants of Health 4
695 - Empowering Pediatric Specialists to Address Health Disparities through Structured Support and Interdisciplinary Collaboration
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 695.4686
Janine Bruce, Stanford University School of Medicine, Stanford, CA, United States; Eimaan Anwar, Boston College Law School, Brighton, MA, United States; DYUTHY RAMACHANDRAN, Stanford University School of Medicine, Cupertino, CA, United States; Emily Trieu, Stanford University School of Medicine, Palo Alto, CA, United States; Noelle Ebel, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States; Noelle Gorka, Stanford University School of Medicine, Stanford, CA, United States; Rebecca Kameny, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States; Kelly Kirby, Lucile Packard Children's Hospital Stanford, Palo Alto, CA, United States; Casey E. Krueger, Stanford University School of Medicine, Belmont, CA, United States; Irene M. Loe, Stanford University School of Medicine, SAN FRANCISCO, CA, United States; Ryan Padrez, Stanford University School of Medicine, Palo Alto, CA, United States; Lisa Chamberlain, Stanford University School of Medicine, Palo Alto, CA, United States

Janine Bruce, DrPH, MPH (she/her/hers)
Senior Research Scholar
Stanford University School of Medicine
Stanford, California, United States
Presenting Author(s)
Background: Health disparities can be addressed via community engagement, policy participation, and policy-relevant research, but few avenues exist to engage pediatric specialists. Departments of Pediatrics are well-positioned to support specialists to address health disparities with guidance from a department-wide Office of Child Health Equity (OCHE).
Objective: To examine pediatric specialists’ perceptions of engagement in structured, coordinated, and interdisciplinary health equity initiatives addressing the unique needs of their patients and families.
Design/Methods: From January to December 2023, the OCHE provided dedicated training and technical assistance to three pediatric divisions (cardiology, developmental-behavioral peds, endocrine/diabetes) interested in engaging in actionable equity initiatives. Participants, referred to as “Health Equity Champions”, included physicians, psychologists, advanced practice providers, and staff. After one year, champions and division chiefs participated in confidential interviews to explore perceptions of engagement. Interviews were transcribed, coded, and team-based theme analysis conducted.
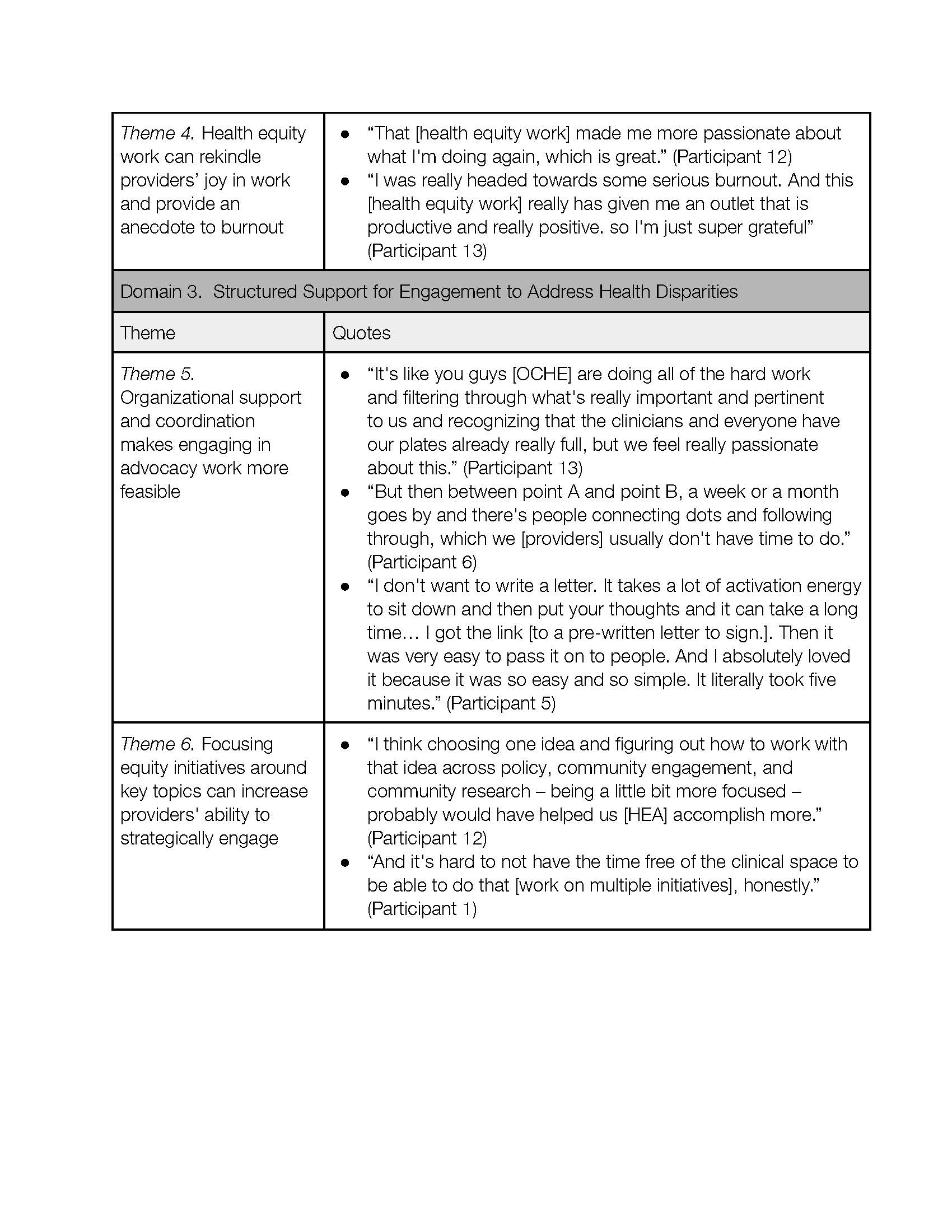
Results: Seventeen specialists were interviewed (n=14 champions; n=3 division chiefs), including champions from cardiology (4 of 7) developmental-behavioral pediatrics (7 of 21), and endocrine/diabetes (3 of 6). The theme analysis resulted in findings across three overarching domains: power of collaboration across divisions, increased job satisfaction, and structured support to address health disparities. Participants reported enjoying improved camaraderie and self-efficacy, reduction in burnout, and increased ability to advocate for patients and empower fellow providers. They attributed this growth to the development of alternative perspectives, rekindling of professional passions, and newfound skills in advocacy to address health disparities. Finally, participants noted how structured OCHE support facilitates engagement, and suggested the need to narrow the focus of initiatives to increase providers' ability to engage strategically (Table 1).
Conclusion(s): The findings from this study underscore the vital role of structured support in fostering pediatric specialists' engagement in equity initiatives. Dedicated training and support through departments of pediatrics can enhance interdisciplinary collaboration across divisions and also cultivate a sense of purpose, essential for addressing health disparities and transforming pediatric practice.
Table 1. Qualitative Themes and Exemplary Quotes (P1)
.jpg)
Table 1. Qualitative Themes and Exemplary Quotes (Cont. P2)