Nephrology 5
Session: Nephrology 5
621 - Factors associated with Kidney Disease Progression in Emerging Adults: Findings from the CKiD Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 621.4879
Rebecca Levy, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Matthew B. Matheson, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States; Michal Melamed, New York University Grossman School of Medicine, New York, NY, United States; Marc Lande, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Susan L. Furth, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Bradley A. Warady, Children's Mercy, Kansas City, MO, United States
- RL
Rebecca Levy, BMBCh (she/her/hers)
Assistant Professor
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Adolescence and young adulthood (AYA) is a period in which patients with kidney disorders require healthcare transitions (HCT) and increasing disease self-management skills in preparation for transfer to new health care providers. Most research in this area has been in the transplant setting; much less is known about health outcomes for patients with chronic kidney disease (CKD) prior to kidney failure.
Objective: We sought to identify potential protective and harmful factors associated with progression of kidney disease and healthcare utilization in this population.
Design/Methods: Evaluation of CKiD cohort, with primary exposure of age (16-18, 19-21, or 22-24 years) and primary outcome of hospitalization. Secondary outcomes consist of need for kidney replacement therapy (KRT) and renin-angiotensin system inhibitor (RAASi) therapy. The unit of observation was study visit; subjects could contribute repeated observations to the analysis. All data was self-reported during a phone or in-person interview. Statistical analysis was conducted by multivariable logistic regression with GEE for repeated measures, with adjustment for potential confounders and testing for interaction between age and other covariates.
Results: Baseline characteristics of the study cohort are shown in Table 1. Notably, fewer adults (participants >18y) reported receiving kidney clinical care in the last year, and increasing age was associated with increasing mental health concerns. In multivariable analysis, the expected effect of increasing age on KRT experience (OR 2.9, CI 1.9-4.4) was ameliorated by living in a large household (Figure 1) which perhaps protected against hospitalization (Figure 2). Although older Black participants were more likely to be prescribed ACEi/ARB disease-modifying therapy compared to their non-Black peers (OR 2.5, CI 1.1-5.6) or younger Black comparators, similar-aged and older teenaged participants identifying as Hispanic were less likely to receive these therapies (OR 0.6, CI 0.4-0.9 for age 19-21; OR 0.3, CI 0.1-0.9 for age 22-24).
Conclusion(s): Large household size is associated with lower rates of kidney disease progression and increased odds of hospitalization in young adults. We hypothesize that this is related to increased family support in young people still living with parents. More work is needed to characterize these patterns and to design interventions to reduce care gaps and poor outcomes.
Table 1
.png) Visit-level time-varying data
Visit-level time-varying dataFigure 1
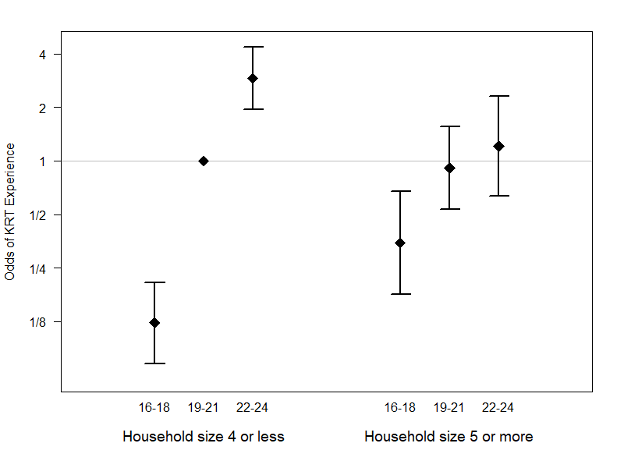 Modification of Kidney Replacement Therapy Risk by Household Size.
Modification of Kidney Replacement Therapy Risk by Household Size.Figure 2
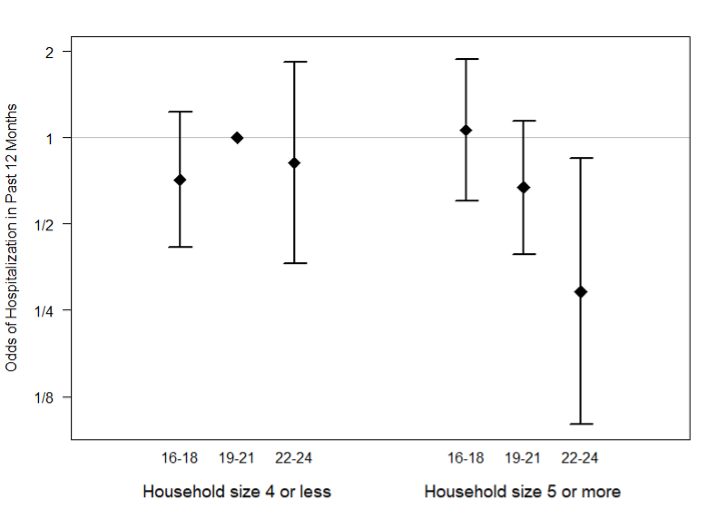 Modification of Hospitalization Risk by Household Size.
Modification of Hospitalization Risk by Household Size.
