General Pediatrics 3
Session: General Pediatrics 3
217 - Evaluation of an early childhood community health worker program at a large public hospital system
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 217.4873
Katherine Piwnica-Worms, NYU Grossman School of Medicine, New York, NY, United States; Rachel Massar, NYU Grossman School of Medicine, New York, NY, United States; Renata Howland, New York University Grossman School of Medicine, New York, NY, United States; Shauntée Henry, NYC Health + Hospitals, New York, NY, United States; Ariel Charney, NYC Health+Hospitals, New York City, NY, United States; Lorraine Kwok, New York University Grossman School of Medicine, New York, NY, United States; Nithya Narayanan, New York University Grossman School of Medicine, Scotch Plains, NJ, United States; John Billings, NYU Robert WagnerSchool of Public Service, New York Ciy, NY, United States; Carolyn A. Berry, New York University Grossman School of Medicine, Maplewood, NJ, United States

Katherine Piwnica-Worms, MD, MHS
Clinical Assistant Professor, Assistant Vice President, Pediatrics
NYU Grossman School of Medicine
New York, New York, United States
Presenting Author(s)
Background: In November 2021, NYC Health + Hospitals (H+H), the nation’s largest public hospital system, implemented an Early Childhood CHW (EC CHW) program across 16 facilities to support families during a critical window of early childhood development. Improving access to and reducing disparities in Early Intervention (EI) is a core program focus, along with social determinants of health, parenting support, and maternal-child wellbeing.
Objective: We conducted a mixed methods evaluation to assess caregiver/staff satisfaction and program impacts.
Design/Methods: Descriptive data was pulled from H+H’s Electronic Medical Records (EMR). Key informant interviews on program implementation were conducted with staff across 5 pediatric clinics, Central Office leadership, and caregivers and analyzed with qualitative methods. Caregiver pre/post surveys (baseline, 3 months) assessed outcomes across the following domains: self-reported health, stress, social needs, parent self-efficacy, engagement in child’s health and development, and program satisfaction. NYS Medicaid claims data identified children (0-36 months) with a CPT-coded well visit at 16 H+H EC CHW sites and citywide comparison sites. A difference-in-difference analysis estimated changes in EI in the treatment and comparison sites before (March 2020-October 2021) and after (April 2022-November 2023) the program started.
Results: EC CHWs reached 23% (18,710) of children 0-5 yrs seen for a well visit at H+H. Staff interviews demonstrated successful program implementation and numerous benefits with actionable facilitators and barriers [TABLE 1]. Self-reported parent engagement in their child’s health care improved significantly and there were positive trends in perceived stress, parenting stress, self-efficacy, and food insecurity [TABLE 2]. For children 12-24 months, increases were greater at H+H sites than citywide controls for EI evaluations (+3.2 percentage point (pp)) and any EI services (+2.1pp) [TABLE 3]. For children 25-36 months, the trend was reversed for EI services (-1.0pp). When results were stratified by race/ethnicity, the EC CHW program was associated with a +3.5pp increase in EI evaluations among Hispanic/Latinx children.
Conclusion(s): Our findings demonstrate that an EC CHW program can have positive effects on self-reported parent engagement and EI utilization for children 12-24 months, possibly augmented for Hispanic/Latinx children. Research is ongoing to examine how EC CHWs can impact healthcare outcomes within Medicaid as a growing number of states invest in CHW workforces.
TABLE 1: Qualitative Key Informant Interview Findings
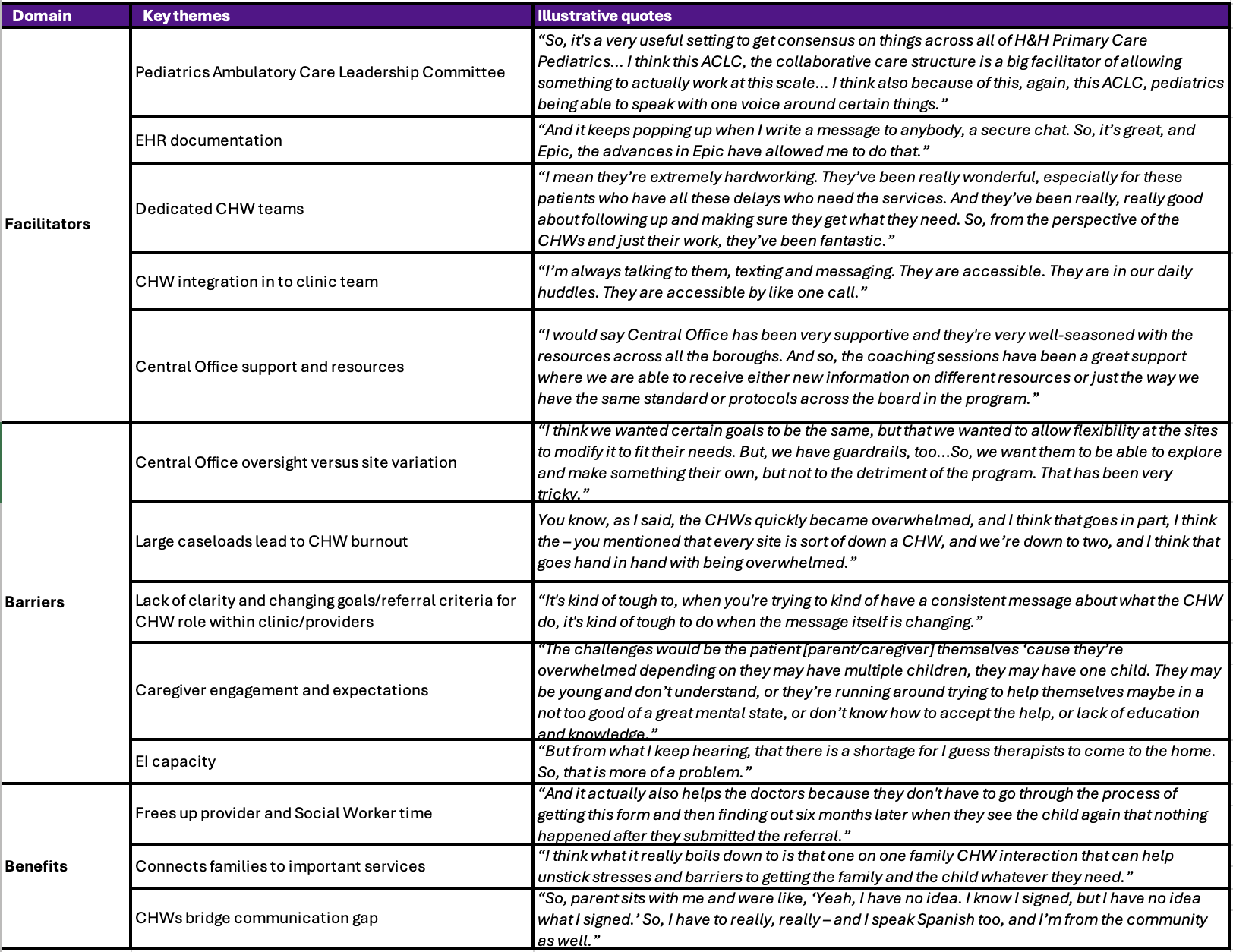 Key informants (N=41) included staff and providers at five pediatric primary care clinics, as well as members of the
Key informants (N=41) included staff and providers at five pediatric primary care clinics, as well as members of the Central Office CHW Pediatric Program leadership team, in order to assess program implementation, with a focus on barriers and facilitators. Interview transcripts were analyzed with a deductive, protocol-driven approach to conduct a rapid qualitative analysis of the interview data. Cross-site findings are organized by theme along with illustrative quotes.
TABLE 2: Caregiver Survey Results, N=115 (88% response rate).
.png) a Test statistics included paired T-test or McNemar test depending on variable structure.
a Test statistics included paired T-test or McNemar test depending on variable structure. b 5-item version of the Short Form Health Survey-8 (SF-8)
c 4-item version of the Perceived Stress Scale-10 (PSS-10)
d Parental Stress Scale (PSS)
e Social needs were measured by a modified version of US Census questions
f Food insecurity defined by the USDA Household Food Security Survey
g Parenting Sense of Competence Scale-5 (PSOC-5)
h Modified version of the Healthcare Self-Efficacy tool
TABLE 3: Pre- and post-period mean percent and difference-in-differences percent change estimates for any Early Intervention (EI) evaluation and services received stratified by age group.
.png) Abbreviations: EI: Early Intervention; DiD: difference-in-difference
Abbreviations: EI: Early Intervention; DiD: difference-in-differenceMedicaid-insured children 0-36 months were attributed to H+H pediatric sites (treatment) based on plurality of well-child visits. Comparison sites include all other NYC providers that were not H+H (and had no known Pediatric CHW program according to NYC Bureau of Early Intervention). The baseline period was from March 2020 - October 2021; the post-period was from April 2022 - November 2023. Children had to have at least 15 months of enrollment across each 20-month period. EI evaluation and services were identified in the Medicaid claims using rate codes [EI Evaluation: 540X-5418; EI Services: 5244, 542X-5485].
We estimate the DiD estimate using linear probability models that include a variable for time (pre/post), treatment, and an interaction between time and treatment, which indicates the effect of the EC CHW program on the outcome.
Data Source: NYS Medicaid claims, 2020-2023

