Health Equity/Social Determinants of Health 5
Session: Health Equity/Social Determinants of Health 5
710 - Chronic Pain, Poverty, and Health Service Use among Children and Youth: An Analysis of Risk and Protective Factors
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 710.4365
Anne E. Fuller, McMaster University, Hamilton, ON, Canada; Jordan Edwards, Hamilton Health Sciences, Hamilton, ON, Canada; Carol Duh-Leong, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Sheri Findlay, McMaster University Michael G. DeGroote School of Medicine, Hamilton, ON, Canada; Allison Rodrigues, McMaster University, Hamilton, ON, Canada; Sandra Westcott, McMaster Universify, Hamilton, ON, Canada; James R. Dunn, McMaster University, Hamilton, ON, Canada; Harriet MacMillan, McMaster University Michael G. DeGroote School of Medicine, Hamilton, ON, Canada; Birken S. Catherine, Sickkids, toronto, ON, Canada; Kathy Georgiades, McMaster University, Ancaster, ON, Canada

Anne E. Fuller, MD, MS (she/her/hers)
Assistant Professor
McMaster University
Hamilton, Ontario, Canada
Presenting Author(s)
Background: Chronic pain is a common manifestation of nervous system activation, often due to interactions of biological and psychosocial factors, including poverty. Service use can be affected by severity of symptoms, as well as contextual risk and protective factors. There is scarce population-representative research studying risk and protective factors for children with chronic pain in the context of poverty.
Objective: Among children and youth with chronic pain: 1) Measure associations between experiences of poverty and health service use; 2) Explore risk and protective factors that may exacerbate or mitigate these associations.
Design/Methods: We used the 2021/22 National Survey of Children’s Health, a cross-sectional survey of US children and families. We included children ages 6 to 17 who had chronic pain in the previous 12 months. Independent variables were poverty in the past year (income < 200% of the federal poverty level) and material hardship since birth. Outcomes were health service use in the previous 12 months for any reason: 1) number of preventive visits (0, 1, >2, with 1 as reference group as standard for this age); 2) any ED visit; 3) any hospital admission. Hypothesized risk factors included diagnosis of depression or anxiety; parenting stress; frustration with health care; foregone health care. Protective factors included family resilience; neighborhood cohesion; family-centered care (FCC). We used adjusted multinomial or logistic regression to measure associations and tested for interactions.
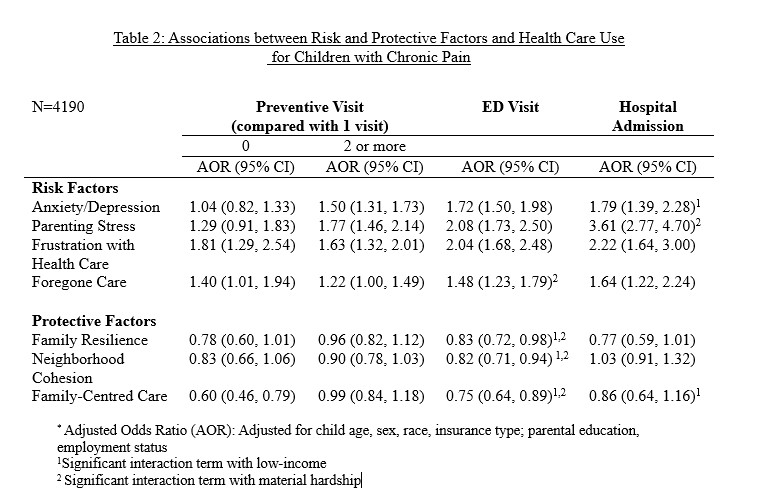
Results: 4868 children were included in the analytic sample (5% of total), with 72% 12 years and older. Poverty and material hardship were associated with higher odds of 0 or > 2 preventive visits and higher odds of ED visit (Table 1). Risk factors were associated with higher odds of each outcome, except 0 preventive visits. Protective factors were associated with lower odds of ED visit; FCC with lower odds of 0 preventive visits (Table 2). There were significant interactions between poverty and all protective factors for ED visits and FCC, anxiety/depression and foregone care for hospital admissions (Table 2). Interactions between poverty and risk/protective factors demonstrated a pattern whereby poverty exacerbated effects of risk factors and reduced effects of protective factors.
Conclusion(s): Among children and youth with chronic pain, exposure to poverty was associated with patterns of service use that suggest barriers to care and higher symptomatology. Risk and protective factors may be affected by poverty, and this should be considered in approaches to preventing and treating chronic pain.
Table 1: Associations between Poverty and Health Care Use for Children with Chronic Pain
.jpg)
Table 2: Associations between Risk and Protective Factors and Health Care Use