Infectious Diseases 6: Infectious diseases syndromes
Session: Infectious Diseases 6: Infectious diseases syndromes
052 - Clinical Characteristics and Management of Pyriform Sinus Fistula Infections in Children
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 52.4357
Shina Tomono, Tokyo Metropolitan Children's Medical Center, Fuchu-shi, Tokyo, Japan; Yuto Otsubo, Tokyo Metropolitan Children's Medical Center, Fuchu, Tokyo, Japan; Yuho Horikoshi, Tokyo metropolitan children's medical center, Fuchu, Tokyo, Japan; Akihiro Shimotakahara, Tokyo Metropolitan Children's Medical Center, Fuchu, Tokyo, Japan; Hiroshi Hataya, Tokyo Metropolitan Children's Medical Center, Fuchu, Tokyo, Japan
- ST
Shina Tomono, MD (she/her/hers)
Resident
Tokyo Metropolitan Children's Medical Center
Fuchu-shi, Tokyo, Japan
Presenting Author(s)
Background: Pyriform sinus fistula (PSF) is an uncommon congenital anomaly that leads to recurrent cervical abscesses and suppurative thyroiditis in children. Limited data are available regarding the clinical characteristics and management strategies for PSF infections in pediatric patients.
Objective: This study aimed to describe the clinical characteristics and therapeutic management of PSF infections in children.
Design/Methods: A retrospective review was conducted, and clinical data of patients with PSF infection were collected from March 2010 to August 2024 in our hospital. Patients under 15 years of age with a diagnosis of PSF infection confirmed by imaging studies and intraoperative findings were included in the study.
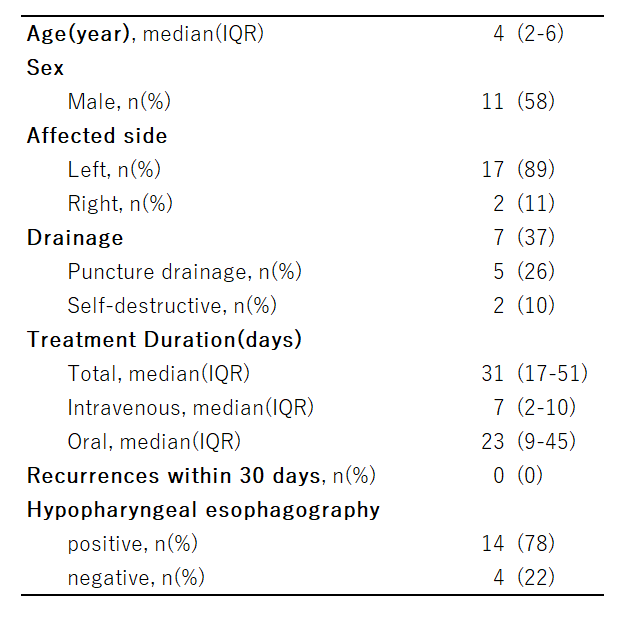
Results: Nineteen cases met the inclusion criteria, with a median age at onset of 4 years (IQR: 2–6), boy’s ratio of 58% and most cases involved left-sided lesions (17 cases, 89%). The total duration of antimicrobial therapy ranged from 7 to 70 days (median 31 days, IQR: 17–51), consisting of 0 to 18 days of intravenous therapy (median 7 days, IQR: 2–10) and 3 to 70 days of oral therapy (median 23 days, IQR: 9–45). Ampicillin-sulbactam was the most used intravenous agent (88%, 14/16 cases), while amoxicillin-clavulanic acid was frequently used as step-down oral therapy (89%, 16/18 cases). Five patients underwent puncture drainage, and two cases experienced spontaneous rupture. Pus cultures grew in three cases, which were Streptococcus mitis, Streptococcus intermedius, and Anaerobic bacteria. No treatment failures or recurrences were observed within 30 days post-treatment. Post-treatment video fluoroscopic swallowing examinations were performed in 18 patients, revealing fistulas in 14 cases. Radical surgical resection was conducted in all but one case, where consent was not obtained. The interval from infection onset to radical surgery ranged from 1 to 40 months (median 5 months, IQR: 3–9).
Conclusion(s): Most pediatric PSF infections were effectively managed with a combination of intravenous and oral antibiotics, typically administered over a duration of 3–4 weeks. All patients achieved favorable clinical outcomes, with no treatment failures or recurrences, regardless of drainage interventions.
Table 1: Summary of 19 patients with PSF infection